
Why Healthcare EHR Modernization Is Accelerating: The Cloud-Native Imperative
August 23, 2025 / Bryan ReynoldsThe Tipping Point for Healthcare IT: Why 60% of Leaders are Modernizing EHRs with Cloud-Native Platforms

The COVID-19 pandemic was more than a global health crisis; it was a crucible for the healthcare industry's digital infrastructure. It stress-tested a decade of IT initiatives, exposing deep, structural fractures in the technological backbone of care delivery. This intense pressure has created an unprecedented mandate for modernization, moving it from a long-term goal to an immediate strategic imperative.
The new executive consensus is clear and backed by data. A landmark 2025 global survey by Deloitte reveals a definitive shift in priorities: 60% of healthcare leaders are now prioritizing investment in core technologies like Electronic Medical Records (EMRs) and Enterprise Resource Planning (ERP) software. This figure is not merely an indicator of a routine upgrade cycle; it represents a fundamental strategic pivot. The industry is moving away from the monolithic, on-premise systems of the past and aggressively embracing agile, cloud-native, and interconnected data platforms.
This article, following the 'They Ask You Answer' approach, will deconstruct this critical trend for B2B executives. It will address the key questions leaders are asking about the powerful drivers, strategic benefits, practical implementation pathways, and crucial financial justifications behind the healthcare modernization imperative.
What's Driving the Urgent Need to Move Beyond Legacy EHR Systems?
For decades, legacy Electronic Health Record (EHR) systems were the bedrock of healthcare's digital transition. Today, they are often the primary obstacle to its future. The decision to modernize is no longer a matter of choice but a strategic necessity for organizational survival, growth, and competitive relevance. The drivers behind this urgency are multifaceted, touching every aspect of the healthcare enterprise from the balance sheet to the bedside.
The Crushing Weight of Technical Debt: A C-Suite Crisis
The concept of "technical debt"—the implied cost of rework caused by choosing an easy, short-term solution over a better, more sustainable approach—has migrated from the IT department to the executive boardroom. In healthcare, this debt has accumulated for years, and the bill is coming due. A staggering 73% of healthcare organizations continue to rely on outdated legacy technologies, leaving them dangerously exposed.
The consequences of this inertia are severe and tangible. They manifest as reduced operational efficiency, a higher probability of medical errors, costly system downtime, and ultimately, compromised care quality. The 2020 cyberattack on Greater Baltimore Medical Center, which was attributed directly to outdated and unpatched equipment, serves as a stark warning of the real-world financial and operational devastation that technical debt can unleash.
The financial burden extends far beyond the risk of a single catastrophic event. The total cost of ownership for legacy systems is a complex and often underestimated drain on resources. A comprehensive analysis of an EHR-to-EHR transition reveals a daunting financial landscape that includes not just the purchase price of a new system but also ongoing maintenance of the old one, exorbitant consulting fees that can be up to ten times the rate of internal analysts, and significant "soft costs" from diverted staff resources and lost revenue when clinicians are pulled away from patient care to participate in IT projects. For large health systems, the total cost of such a transition can easily range from $250 million to over $1 billion.
This reality has fundamentally shifted the conversation around IT investment. Technical debt is no longer an operational headache for the CIO; it has become a primary financial risk for the CFO. The logic is inescapable: outdated systems directly increase the risk of catastrophic financial events like ransomware attacks, which can halt operations for weeks. This elevated risk profile, in turn, impacts cybersecurity insurance premiums. Furthermore, data breaches resulting from legacy vulnerabilities can lead to massive regulatory fines under HIPAA. When these direct financial risks are combined with the immense, often hidden, costs of maintaining and transitioning from these systems, it becomes clear that technical debt is a balance sheet liability. This transforms the modernization decision from a simple IT budget item into a shared strategic imperative co-owned by the CFO and the CIO, focused on mitigating quantifiable financial risk.

Interoperability Failure: The High Cost of Data Silos
Perhaps the most profound failure of the legacy EHR era is the systemic lack of interoperability. A patient's medical history is often scattered across dozens of disconnected, proprietary systems, creating a fragmented and incomplete view of their health journey. This is not a mere inconvenience; it is a critical flaw in the care delivery model that leads directly to diagnostic delays, dangerous miscommunications, redundant and costly testing, and missed opportunities for early intervention.
The challenges are deeply embedded within the technology and the market that created it. A lack of universal data standardization means that different systems record and define the same clinical concept in incompatible ways. Vendor lock-in, achieved through proprietary software, creates closed ecosystems that actively discourage data exchange with competing platforms. Even where standards like HL7 and Fast Healthcare Interoperability Resources (FHIR) exist, their fragmented and inconsistent adoption across organizations creates a complex web of incompatibility that perpetuates the problem of isolated data silos.
The Human Cost: Clinician Burnout and the Workforce Crisis
The negative impact of legacy systems extends beyond technology and finance; it directly affects the industry's most valuable asset: its people. The clunky interfaces, tedious manual data entry, and the shifting of clerical work onto clinicians were hallmarks of early EHR implementations and are now recognized as a major contributor to professional burnout. This is an existential threat to a sector where over 80% of executives cite workforce shortages and hiring difficulties as a top challenge.
When leaders of existing EHR-based systems are surveyed, they consistently identify "resistance to change" from clinical staff as their single biggest implementation challenge. This resistance is often misinterpreted as a simple aversion to new technology. In reality, it is a rational response from professionals who are being asked to adapt their highly refined clinical workflows to poorly designed systems that disrupt, rather than enhance, patient care.
This direct link between technology and talent makes EHR modernization a critical workforce retention strategy. The causal chain is clear: clinician burnout is a primary driver of the healthcare workforce crisis, leading to high turnover and soaring recruitment costs. Poorly designed, non-interoperable legacy EHRs are a significant source of daily frustration and a direct cause of that burnout. Therefore, investing in a modern, user-friendly, and interoperable clinical platform is not merely an IT project; it is a direct and powerful investment in the well-being and stability of the clinical workforce. For CFOs and Chief Operating Officers concerned with operational continuity and labor costs, the ROI can be measured in reduced staff turnover, lower hiring expenses, and higher productivity—a compelling business case for change.
The Rise of Patient Consumerism
The final driver is the patient. Modern consumers, accustomed to the seamless, on-demand, and personalized digital experiences offered by the retail, banking, and entertainment industries, now bring those same expectations to their healthcare journey. An overwhelming majority—over 80%—of consumers now expect their healthcare providers to leverage digital technologies to enhance their care experience. Legacy systems, with their conspicuous absence of user-friendly patient portals, mobile access, and transparent data sharing, are fundamentally misaligned with this new paradigm. For providers who fail to adapt, this creates a significant competitive disadvantage in a market where patient choice is increasingly influential.
Why is the Cloud the Inevitable Future for Healthcare Data?
As healthcare executives confront the limitations of legacy systems, they are overwhelmingly turning to one solution: the cloud. The migration of healthcare data and applications to cloud-native platforms is no longer a niche trend but an industry-wide inevitability. This shift is driven by a powerful convergence of factors that deliver unparalleled agility, security, financial efficiency, and the foundational architecture required for the next generation of healthcare innovation.
Beyond Storage: Achieving Agility, Scalability, and Resilience
The pandemic provided the ultimate proof of concept for the cloud's strategic value. As health systems were forced to scale virtual care offerings and data exchange capabilities almost overnight, the elastic, pay-as-you-go flexibility of cloud-based services proved indispensable—a feat that would have been impossible with rigid on-premise infrastructure. Modern cloud infrastructure empowers organizations to innovate without the constraints of traditional systems, with the ability to scale resources automatically to meet the unpredictable peaks and troughs of demand.
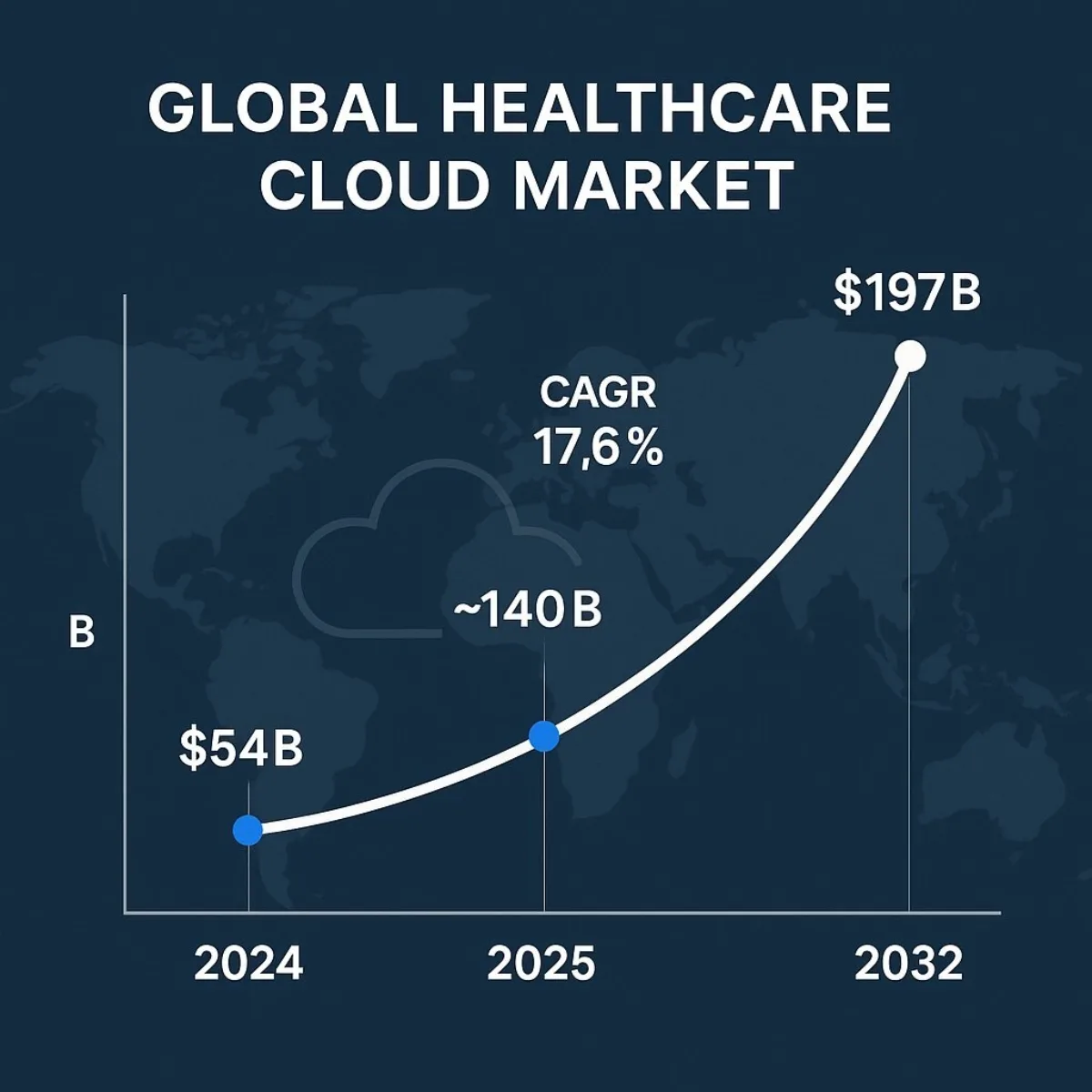
This capability has driven near-universal adoption. Today, over 94% of enterprise organizations utilize the cloud for a significant portion of their workloads. This trend is particularly pronounced in healthcare, where the global cloud computing market is projected to experience explosive growth, surging from
USD 54.28 billion in 2024 to an estimated USD 197.45 billion by 2032 , reflecting a compound annual growth rate (CAGR) of 17.6%.
A critical, and often overlooked, benefit of this migration is a dramatic improvement in organizational resilience. Cloud platforms provide sophisticated, geographically distributed disaster recovery capabilities "out of the box." This enables robust data backup and automated failover to different data centers, significantly reducing the risk of the catastrophic downtime from cyberattacks or natural disasters that puts patient safety and operational continuity at stake.
The Inversion of the Security Paradigm
For years, the prevailing wisdom in healthcare IT was that sensitive patient data was safest when kept on-premise, behind the organization's own firewalls. Today, that paradigm has been completely inverted. In a remarkable shift in perception, a full 60% of healthcare leaders now cite enhanced security as one of the top benefits of moving to the cloud .
This change is rooted in the reality of the modern cybersecurity landscape. Major cloud providers like Microsoft Azure and Amazon Web Services (AWS) have invested billions in developing enterprise-grade, multi-layered security architectures that far exceed the capabilities of all but the largest and most sophisticated in-house IT teams. These platforms employ state-of-the-art data encryption both at rest and in transit, granular role-based access controls, and vast, AI-driven automated threat detection networks. Furthermore, they come with a portfolio of built-in compliance certifications for rigorous standards like HIPAA, GDPR, and HITRUST, simplifying the complex regulatory burden for healthcare organizations.
The Compelling Financial Case: From CapEx to Strategic OpEx
The adoption of cloud infrastructure fundamentally transforms the financial model of healthcare IT. It marks a strategic shift away from massive, upfront capital expenditures (CapEx) on servers, storage, and data center facilities. Instead, it moves to a predictable, subscription-based operational expenditure (OpEx) model where organizations pay only for the resources they consume.
This pay-as-you-go approach eliminates the high, often unpredictable, costs of legacy system maintenance, hardware refreshes, and the brittle, one-off integrations required to keep outdated systems running. The financial impact is significant. Independent analysis has found that moving workloads to the public cloud can lead to a Total Cost of Ownership (TCO) reduction of 30-40%. This financial efficiency is not just about cost-cutting; it frees up capital that can be reallocated from basic infrastructure maintenance toward strategic, value-adding initiatives in innovation, patient experience, and care delivery.
The Foundation for Future Innovation
While the operational and financial benefits are compelling, the most profound reason for migrating to the cloud is strategic: it is the non-negotiable prerequisite for participating in the future of healthcare. Transformative technologies like artificial intelligence, machine learning, and generative AI—which are set to redefine everything from diagnostics to drug discovery—require the immense computing power, vast data storage, and elastic scalability that only cloud platforms can provide.
The cloud enables the creation of a "digital core," a unified data platform that finally breaks down the organizational silos that have long blocked advanced analytics. It provides the API-driven architecture necessary to seamlessly integrate with a growing ecosystem of partners, from specialized software vendors to medical device manufacturers. This connected foundation is essential for enabling high-value use cases like real-time population health analytics, accelerating clinical research, and delivering truly personalized medicine.
The strategic imperative for this shift has evolved. While early cloud adoption narratives focused heavily on TCO reduction, the conversation at the executive level is now dominated by the promise and challenge of AI. With 78% of organizations now reporting the use of AI, leaders understand that this technology is the next competitive frontier. The technical reality is that meaningful AI and machine learning at scale are impossible without the unified data and massive computational power of the cloud. Therefore, health systems are not just moving to the cloud to save money on servers; they are migrating because they recognize that failing to do so means being locked out of the next generation of healthcare innovation. The cloud has become the entry ticket to the AI era.
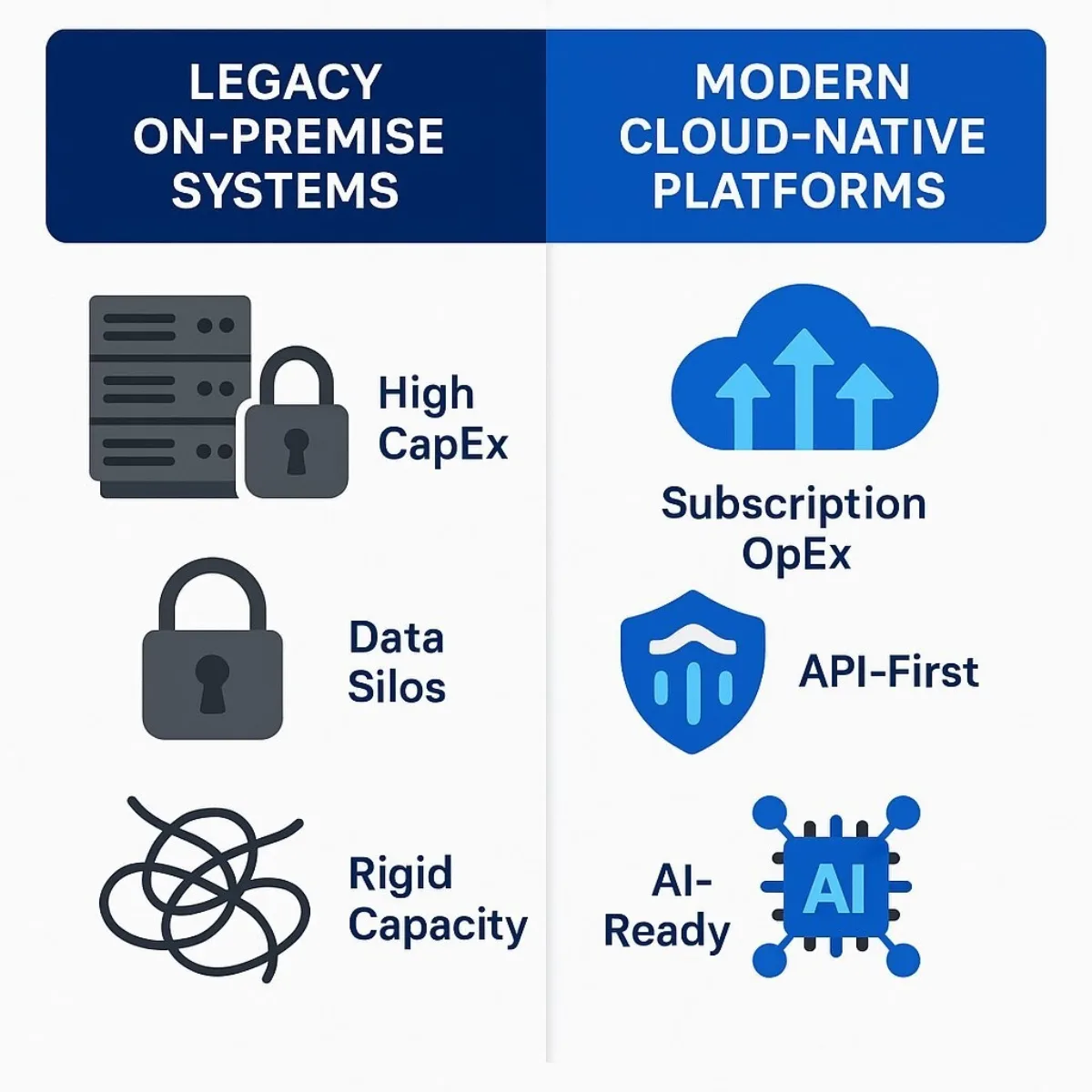
| Feature | Legacy On-Premise Systems | Modern Cloud-Native Platforms |
|---|---|---|
| Cost Model | High Upfront CapEx; Unpredictable maintenance & upgrade costs | Subscription-based OpEx; Predictable, pay-as-you-go model |
| Scalability | Fixed capacity; Scaling requires costly hardware procurement | Elastic; Scales automatically with demand; "Limitless capacity" |
| Security | Sole responsibility of in-house IT; Vulnerable to outdated patches | Shared responsibility model with specialized provider; Advanced, automated security |
| Interoperability | Often proprietary and siloed; Requires complex, brittle integrations | API-first architecture; Built on open standards like FHIR |
| Innovation | Stifled by rigid architecture; Cannot support modern AI/ML workloads | Foundation for AI, telehealth, and advanced analytics; Faster deployment cycles |
| Resilience | Dependent on local disaster recovery plans; High risk of downtime | Geographically distributed data centers; Automated failover and recovery |
What Does a Successful EHR Modernization Strategy Actually Look Like?
Embarking on an EHR modernization journey requires a clear, pragmatic strategy that balances technological ambition with operational reality. A successful approach moves beyond outdated paradigms, embraces a modern technology stack, and recognizes the critical role of expert partners in navigating the complexities of transformation.
Beyond 'Rip and Replace': Phased Modernization for Minimal Disruption
The notion of a single, "big bang" replacement of a core EHR system is often fraught with unacceptable levels of risk, cost, and operational disruption. A far more pragmatic and increasingly common approach is a phased, modular modernization strategy. This allows an organization to achieve incremental value, manage change effectively, and minimize the impact on clinical workflows. A 2023 Deloitte study found that such a phased approach, often starting with high-risk backend systems, can lead to a 25-40% reduction in IT operational costs over three years with minimal service interruption.
Common modernization pathways include :
- Rehosting (Lift-and-Shift): This involves migrating an application to a cloud infrastructure with minimal changes to its code. It's the fastest path to realizing the benefits of cloud infrastructure, such as improved scalability and resilience, without re-engineering the application itself.
- Replatforming: This approach involves making targeted cloud-specific optimizations to an application to improve performance or efficiency, but without changing its core architecture. This might include moving from a self-managed database to a managed cloud database service.
- Refactoring/Rearchitecting: This is a more intensive process of redesigning and restructuring parts of the application to be truly cloud-native. This often involves breaking down a large, monolithic application into smaller, more manageable components.
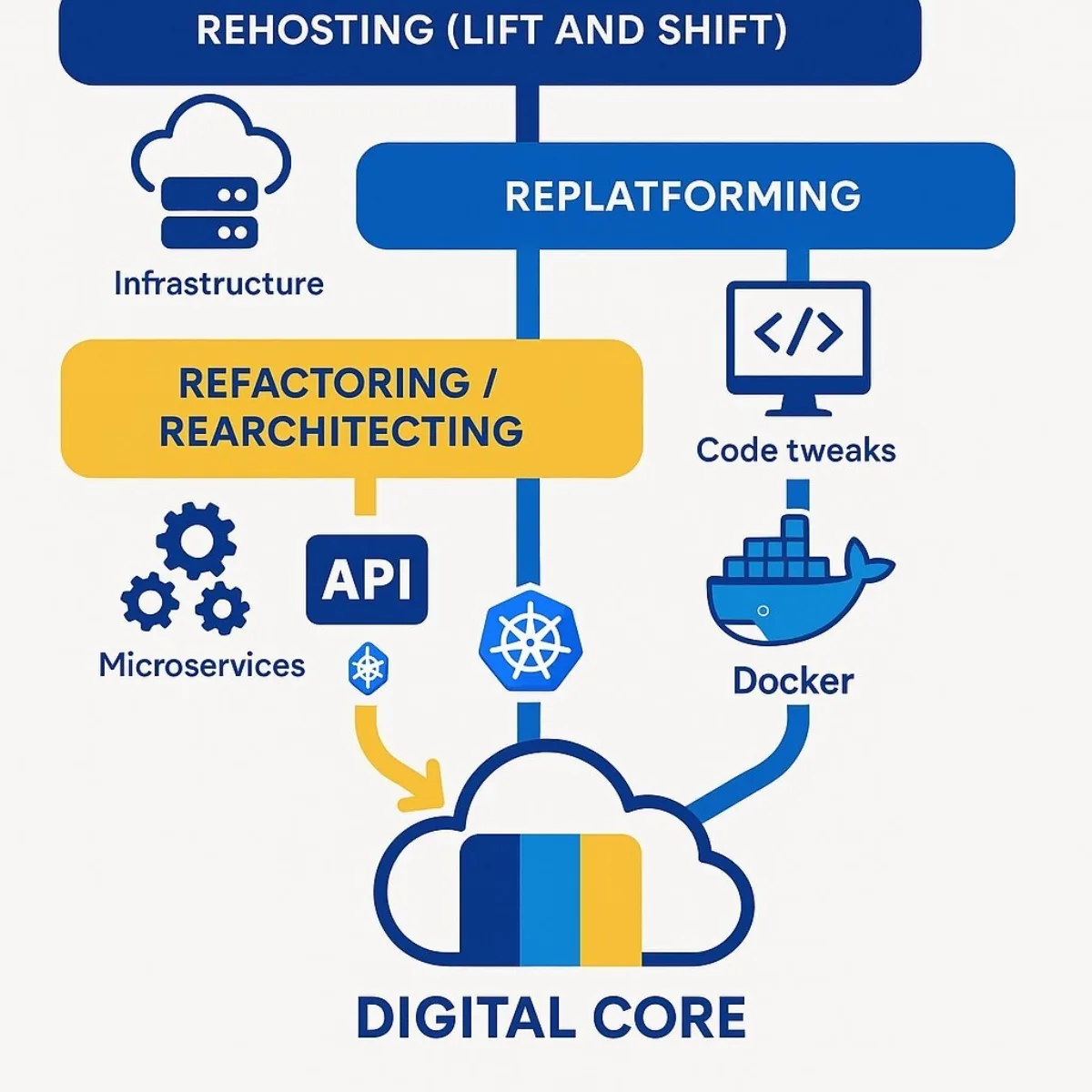
The Modern Technology Stack: Building a 'Digital Core'
At the heart of a modern healthcare IT strategy is the creation of a "digital core"—an interoperable, secure, and scalable set of systems built on modern standards and architectures.
- APIs as the Lingua Franca: The key to unlocking data from legacy silos is the widespread use of Application Programming Interfaces (APIs). In healthcare, the Fast Healthcare Interoperability Resources (FHIR) standard has emerged as the universal language for data exchange. FHIR-based APIs allow disparate systems to communicate seamlessly and securely, forming the connective tissue of a modern health ecosystem.
- Microservices and Containerization: The practice of refactoring involves breaking down monolithic legacy applications into a collection of smaller, independent "microservices." Each service handles a specific business function and can be developed, deployed, and scaled independently. These services are often packaged in "containers" using technologies like Docker , which encapsulates the application and its dependencies, making it highly portable and efficient. To manage these containers at scale, the industry has standardized on orchestration platforms like Kubernetes , which automate the deployment, scaling, and management of containerized applications. This modular architecture dramatically improves system resilience; if one microservice fails, it doesn't bring down the entire system, a critical feature for mission-critical clinical applications.
Case Study in Focus: Jefferson Health's Migration of Epic to Microsoft Azure
The journey of Jefferson Health, a multi-state nonprofit network of hospitals, provides a powerful real-world blueprint for large-scale EHR modernization. As one of the largest U.S. providers to migrate its core Epic EHR system to the public cloud, their strategy offers valuable lessons.
- Strategic Goals: Jefferson Health's decision was driven by three key business objectives: achieving greater business agility to seamlessly integrate newly acquired hospitals into their Epic instance; enhancing resiliency through robust disaster recovery and business continuity; and building a foundation for innovation to leverage the advanced AI and machine learning capabilities of the Azure platform.
- Implementation: The project was a strategic partnership with Microsoft and the consulting firm Accenture. They leveraged Microsoft Azure's purpose-built reference architecture, which is optimized for Epic workloads. Crucially, the migration was viewed as more than just a technical "lift and shift"; it was a strategic opportunity to implement contemporary cybersecurity controls, harden systems, and enforce data encryption from the ground up.
- Outcome: The move to Azure delivered immediate advantages in business continuity and risk mitigation. More importantly, it positioned Jefferson Health for the future, creating an elastic and powerful platform that allows them to "turn on" and leverage advanced AI capabilities in short order, accelerating their path to data-driven healthcare.
The market momentum behind such moves is undeniable, reflecting a massive, industry-wide shift away from on-premise infrastructure.
| Year | Projected Market Size (USD Billions) |
|---|---|
| 2024 | $54.28 |
| 2025 | $63.55 |
| 2030 | ~$140 (Interpolated) |
| 2032 | $197.45 |
Data synthesized from market reports. The market is projected to grow at a CAGR of 17.6%, signaling a definitive shift to cloud-based platforms.
The Critical Role of Custom Development: Introducing Baytech Consulting
While powerful off-the-shelf cloud platforms like Microsoft's Azure Health Data Services provide an essential foundation for modernization, they are not a complete, turnkey solution. The true value of a modern platform is unlocked by seamlessly connecting this new digital core to the organization's unique and complex ecosystem. This includes legacy systems that cannot be immediately replaced, third-party SaaS applications, a growing network of Internet of Medical Things (IoMT) devices, and custom patient-facing portals and mobile apps.
This integration represents the critical "last mile" of modernization, and it requires deep, specialized expertise in custom software development, like those found in custom enterprise application architecture. This is precisely the role that a firm like Baytech Consulting occupies. They specialize in designing and building the bespoke APIs, secure data pipelines, and custom applications that create a truly unified and interoperable system. Baytech Consulting bridges the gap between a cloud platform's potential and an organization's specific operational reality, ensuring that data flows seamlessly, securely, and intelligently to the point of care, decision, or insight.
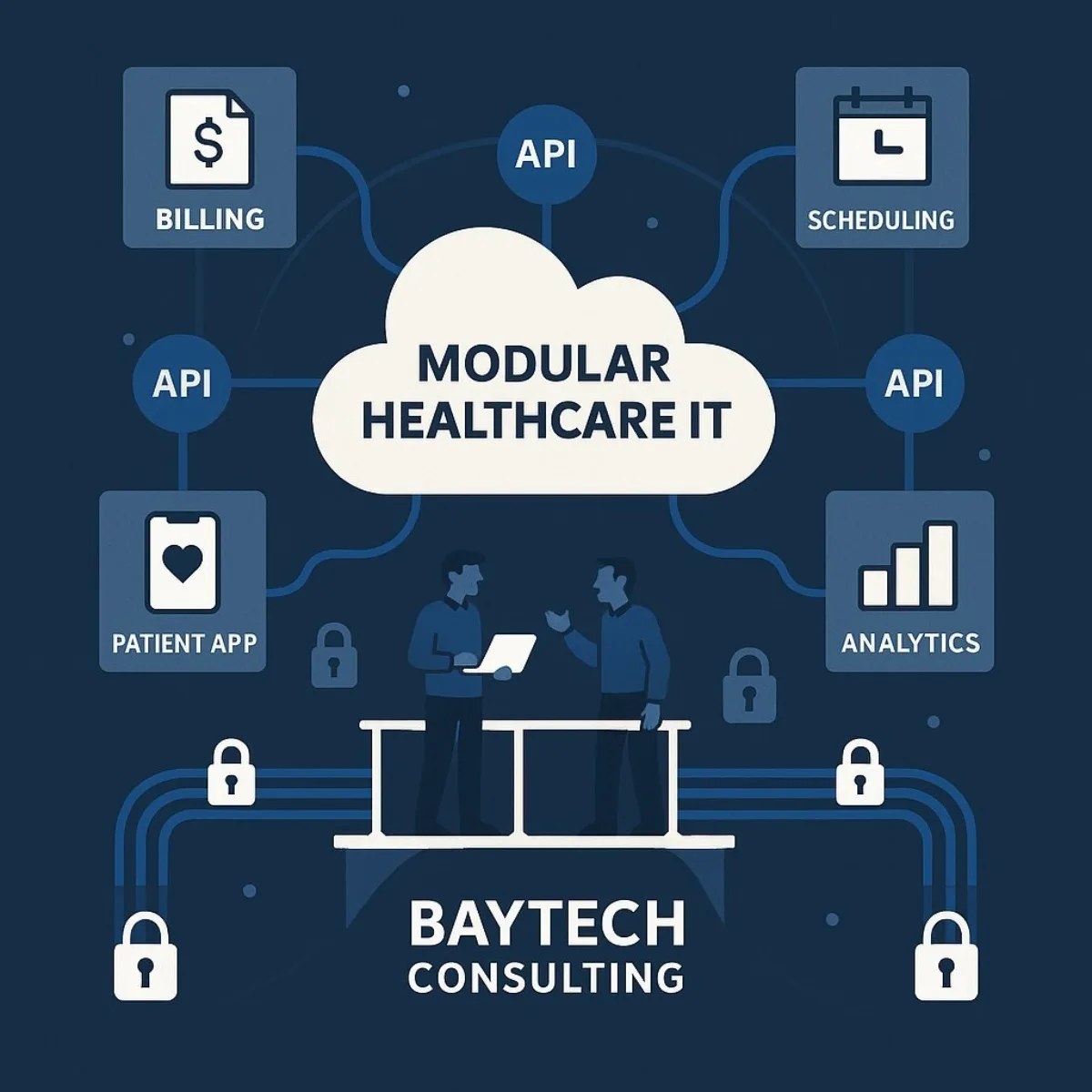
This integration layer is becoming the most strategic component of the modern healthcare IT stack. The very concept of a single, monolithic "EHR" is dissolving. It is being replaced by a "composable healthcare enterprise," where the core EHR is just one modular component in a broader, API-driven digital ecosystem. The emphasis is shifting from a single vendor to a unified data hub that can ingest information from multiple sources. In this new model, functionality is unbundled from the core system and delivered through smaller, best-of-breed tools for scheduling, billing, telehealth, and analytics, all communicating via standardized APIs. This means the future isn't about finding one perfect EHR; it's about building an agile platform where the best tools can be "plugged in." This elevates the API strategy and the custom integration work—the specialty of Baytech Consulting—to a position of paramount strategic importance, arguably more critical than the choice of the core EHR vendor itself.
How Do We Justify the Investment and Ensure Executive Alignment?
A successful modernization initiative is as much about building a sound business case and fostering executive alignment as it is about implementing the right technology. For a project of this scale and strategic importance, the partnership between financial and technology leadership is paramount.
Forging the CFO-CTO Alliance
In the current era of digital transformation, the traditional, often siloed, relationship between the Chief Financial Officer (CFO) and the Chief Technology Officer (CTO) is obsolete. Technology is no longer a peripheral cost center but a primary engine of strategic growth, operational efficiency, and risk management. As such, the collaboration between the CFO and CTO has never been more critical. CFOs must evolve from being purely financial stewards to becoming active and informed participants in major technology decisions.
Achieving this requires a commitment to open, frequent, and substantive communication. The goal is to create a shared language and a unified understanding of how technology investments align with overarching financial priorities, core business goals, and evolving customer needs. This partnership ensures that technology strategy is not developed in a vacuum but is instead woven into the financial and strategic fabric of the organization.
Redefining ROI: Beyond TCO and into Value-Based Outcomes
The business case for EHR modernization cannot rest on IT cost savings alone. While a reduction in Total Cost of Ownership (TCO) is an important benefit, the true, transformative value of the investment is realized in how it impacts broader business and clinical objectives. The justification must therefore be built on a more holistic and strategic definition of Return on Investment (ROI).
A modern framework for evaluating this investment should include:
- Clinical Value: Measurable improvements in patient outcomes driven by better, more timely access to complete data; a reduction in medical errors; and the enablement of predictive analytics for early intervention.
- Operational Value: Tangible gains in clinician productivity through streamlined workflows; a reduction in the administrative burden that contributes to burnout; and higher staff retention rates, which lowers recruitment and training costs.
- Financial Value: Enhanced success in value-based care contracts, which are fundamentally data-dependent; improved revenue cycle management through better data accuracy and automation; and the critical mitigation of multi-million dollar security breaches and regulatory fines.
- Patient Value: Higher patient satisfaction and engagement scores, which are increasingly tied to an organization's reputation, patient loyalty, and market share in a competitive landscape.

Shared Responsibility for a Data-Driven Future
EHR modernization is not an IT project; it is an enterprise-wide transformation. Its success hinges on a culture of shared responsibility that extends across all stakeholders, including technology vendors, internal IT departments, and, most importantly, the clinical and administrative staff who will use the new systems every day.
From a governance perspective, this requires C-suite leadership to establish clear and robust policies for data access, usage rights, and patient consent management in this new, more open environment. It also demands a forward-looking approach to technology investments, ensuring that the chosen platforms and architectures are scalable, adaptable, and future-proofed to accommodate the rapid pace of technological change.
Ultimately, the most compelling business case for EHR modernization reframes the expenditure entirely. It is not a cost to be minimized, but rather a crucial strategic investment that acts as a hedge against the five greatest threats to a modern health system's viability: catastrophic cybersecurity breaches, unsustainable clinician turnover, a poor patient experience that erodes loyalty, failure to compete in a value-based care environment, and non-compliance with evolving interoperability mandates. The research clearly shows that a modern, cloud-based, interoperable system is a direct mitigator for each of these major board-level risks. By framing the discussion in these terms, the conversation shifts from "How much will this cost?" to the far more urgent question: "What is the cost of inaction across all of our most critical strategic vulnerabilities?" This holistic justification provides a powerful and unified rationale for decisive executive action.
Conclusion: Your Roadmap to a Connected, Data-Driven Future
The evidence is clear and overwhelming. The convergence of rising patient expectations, unprecedented workforce pressures, regulatory mandates for interoperability, and the dawn of the AI era has transformed EHR modernization from a future consideration into an immediate and urgent strategic imperative. In this new landscape, maintaining the status quo with legacy systems is no longer a financially prudent choice but a high-risk gamble against the future viability of the organization.
The path forward begins with a foundational commitment to a cloud-native, API-first architecture. This is the essential first step that unlocks the business agility required to compete, strengthens security to mitigate existential threats, and paves the way for a more intelligent, predictive, and personalized model of care delivery.
This transformation, however, is inherently complex. It requires not only the right technology platforms but also the right strategic partners. For the critical "last mile" work of custom integration, data pipeline engineering, and bespoke application development that brings a modern digital ecosystem to life, partnering with a specialist firm can be the decisive factor. An expert partner like Baytech Consulting provides the deep technical expertise needed to bridge the gap between platform potential and operational reality, ensuring a successful transformation that delivers lasting value. For a closer look at how custom software is transforming patient engagement, operational efficiency, and ROI in healthcare, explore our guide to digital-first patient experience and custom healthcare software.
Supporting Links
- Deloitte's 2025 Global Health Care Outlook: https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-global-health-care-executive-outlook.html
- The CMS Interoperability Framework: https://www.cms.gov/newsroom/press-releases/white-house-tech-leaders-commit-create-patient-centric-healthcare-ecosystem
- The HL7 FHIR Standard Official Website: https://www.hl7.org/fhir/
- AI in Healthcare 2025: Market Growth, Benefits & the Strategic Edge for Business Leaders: https://www.baytechconsulting.com/blog/ai-in-healthcare-2025
- How Digital-First Software is Transforming Patient Engagement & ROI in Healthcare: https://www.baytechconsulting.com/blog/digital-first-patient-experience-healthcare
- How Custom Software Solves Manufacturing’s Supply Chain Crisis: https://www.baytechconsulting.com/blog/custom-software-manufacturing-supply-chain-crisis
About Baytech
At Baytech Consulting, we specialize in guiding businesses through this process, helping you build scalable, efficient, and high-performing software that evolves with your needs. Our MVP first approach helps our clients minimize upfront costs and maximize ROI. Ready to take the next step in your software development journey? Contact us today to learn how we can help you achieve your goals with a phased development approach.
About the Author

Bryan Reynolds is an accomplished technology executive with more than 25 years of experience leading innovation in the software industry. As the CEO and founder of Baytech Consulting, he has built a reputation for delivering custom software solutions that help businesses streamline operations, enhance customer experiences, and drive growth.
Bryan’s expertise spans custom software development, cloud infrastructure, artificial intelligence, and strategic business consulting, making him a trusted advisor and thought leader across a wide range of industries.


