
AI in Healthcare 2025: Market Growth, Benefits & the Strategic Edge for Business Leaders
August 03, 2025 / Bryan ReynoldsThe AI Revolution in Healthcare: Your 2025 Guide to Transformation, Benefits, and Real-World Impact
Introduction: Beyond the Hype—What Does AI in Healthcare Really Mean?
The term "AI in healthcare" is everywhere, promising a future of automated diagnoses, robotic surgeons, and hyper-personalized medicine. For business leaders, the constant buzz can be deafening, making it difficult to separate science fiction from strategic reality. The core questions remain: How is Artificial Intelligence actually transforming the healthcare industry today? What are the tangible benefits, the real-world applications, and what does this seismic shift mean for your business?
This guide cuts through the noise to provide a clear, data-driven analysis for executives focused on the business implications of technology. It is a comprehensive, no-nonsense look at the state of AI in healthcare in 2025. To deliver on this promise, this report will tackle the tough questions head-on: Is AI truly improving patient care? Is it replacing doctors? What are the critical risks and challenges, from algorithmic bias to data security, that must be managed? By addressing these questions with transparency and robust data, this analysis will equip you with the strategic insights needed to navigate one of the most significant technological transformations of our time.
1. The Unstoppable Growth of AI in Healthcare: A Market Snapshot
The adoption of AI in healthcare is not a speculative trend; it is a market reality backed by massive financial momentum. This growth is not merely a product of technological curiosity but a strategic response to deep, systemic pressures facing the global healthcare industry. For business leaders, understanding the scale and velocity of this market is the first step in grasping the opportunities and imperatives it presents.
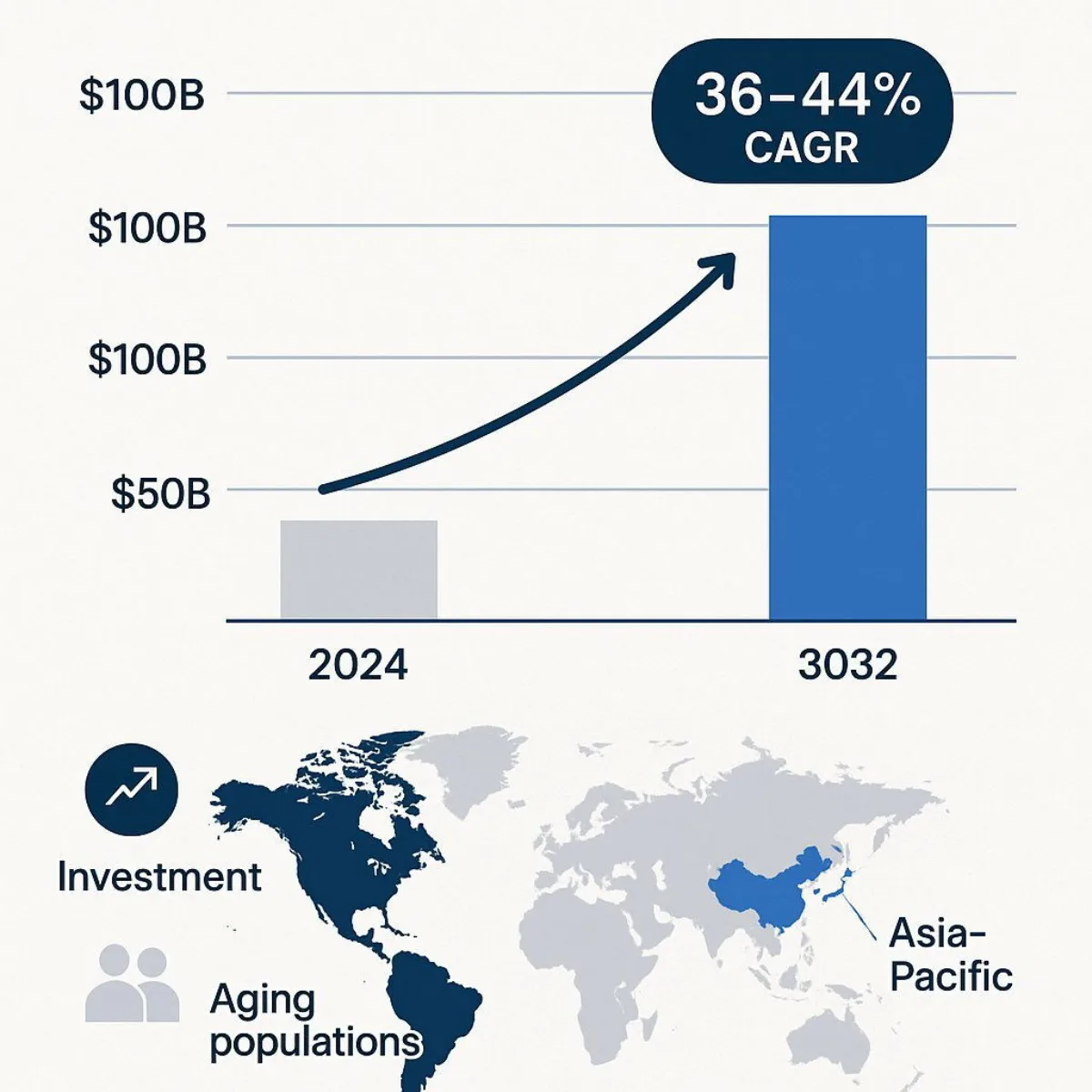
Market analysts project the global AI in healthcare market, valued between $14.9 billion and $29.0 billion in 2024, to experience explosive growth over the next decade. Forecasts indicate the market will skyrocket to over $110 billion by 2030, with some projections reaching as high as $504 billion by 2032. This trajectory is powered by a blistering Compound Annual Growth Rate (CAGR) estimated to be between 36% and 44% from 2025 onward, signaling a period of intense investment and rapid innovation. The sheer variance in these long-term forecasts—from a conservative $110 billion to an aggressive $504 billion—does not indicate a lack of clarity. Instead, it highlights the market's immense volatility and massive upside potential. This range suggests a market that is still defining its own boundaries, where new categories can be created and entire segments are ripe for disruption—a critical signal for any strategist or investor.
This explosive growth is fueled by a confluence of powerful drivers:
- Systemic Pressures: Healthcare systems worldwide are grappling with the rising need for early disease detection, intense pressure to reduce soaring costs, and the immense challenge of serving an aging global population. The UN projects the number of people aged 65 or older will double by 2050, straining resources and demanding more efficient care models. AI is increasingly viewed not as a luxury but as a necessary tool to manage these fundamental crises.
- The Data Deluge: The healthcare industry is on track to generate over 10 trillion gigabytes of data in 2025. This includes everything from electronic health records (EHRs) and medical imaging to genomic sequences and data from wearable devices. This sheer volume of complex, often unstructured data is impossible for humans to analyze effectively, creating a critical need for AI algorithms that can identify patterns and derive actionable insights.
- Surging Investment: Governments and private enterprises are pouring capital into healthcare AI. This funding is a major catalyst, supporting the R&D needed to develop innovative solutions. For example, the Indian health-tech startup MedMitra AI recently secured significant funding to develop autonomous AI solutions aimed at making care more precise and personalized, illustrating a global trend of investment in the space.
Geographically, North America currently dominates the market, accounting for approximately 49% to 54% of the global share due to its advanced healthcare infrastructure and high adoption rates of new technologies. However, the Asia-Pacific region is projected to be the fastest-growing market, driven by a rising geriatric population, increasing medical tourism, and accelerated research activities in countries like China, Japan, and India.
| Year | Market Size (Low Estimate in USD) | Market Size (High Estimate in USD) | Projected CAGR |
|---|---|---|---|
| 2024 | $14.92 Billion | $29.01 Billion | - |
| 2025 | $21.66 Billion | $39.25 Billion | 36% - 44% |
| 2030 | $110.61 Billion | $173.55 Billion | 36% - 44% |
| 2032 | - | $504.17 Billion | 36% - 44% |
Data synthesized from multiple market reports to show a credible range.
Ultimately, the market data reveals a crucial narrative: AI is being adopted out of necessity. The technology is not just an innovative tool for forward-thinking organizations; it is becoming a strategic imperative for any healthcare entity looking to remain viable in a system under immense strain. This reframes AI from a "nice-to-have" tech upgrade to a "must-have" solution for core business challenges like cost control, operational efficiency, and service delivery.
2. What Are the Key Benefits of AI in Healthcare? A Three-Pillar Framework
The immense investment flowing into healthcare AI is driven by a clear and compelling value proposition. The benefits can be organized into a simple, powerful framework of three core pillars: enhancing clinical precision, slashing operational costs, and personalizing patient care. For executives, this framework provides a clear way to understand and communicate the multifaceted impact of AI.
Pillar 1: Supercharging Diagnostics and Clinical Accuracy
Perhaps the most mature and impactful application of AI in healthcare today is its role as a "second pair of eyes" for clinicians, particularly in medical imaging. AI algorithms excel at analyzing complex visual data from X-rays, CT scans, and MRIs, identifying subtle patterns that may be missed by the human eye. This capability is not theoretical; it is delivering quantifiable improvements in diagnostic accuracy.
- Dominance in Radiology: The data shows that medical imaging is a clear leader in AI adoption. An estimated 76% of all AI-enabled medical devices authorized for sale in the US are used in radiology.
- Quantifiable Accuracy Gains: The statistics are striking. AI has demonstrated the ability to rule out heart attacks with 99.6% accuracy—twice as fast as human clinicians. In oncology, AI models developed at Massachusetts General Hospital and MIT achieved 94% accuracy in detecting lung nodules, compared to just 65% for human radiologists. Furthermore, AI has been shown to detect 64% of epilepsy brain lesions that were previously missed by experts.
- Real-World Validation: These accuracy gains are being validated in clinical settings. A notable early value assessment by the UK's National Institute for Health and Care Excellence (NICE) for the AI tool AZtrauma found that when clinicians used the software to detect bone fractures, their mean sensitivity jumped from 86.5% to 95.5% without any significant loss of specificity.
Pillar 2: Slashing Operational Costs and Administrative Burden

While advanced diagnostics capture headlines, AI's most immediate financial impact may come from tackling the "hidden drag" on the healthcare system: administrative waste. Healthcare professionals report spending as much as 34% of their time on administrative tasks, a major driver of clinician burnout, inefficiency, and soaring costs. AI-powered automation directly targets this problem by streamlining routine workflows.
- Automating the Back Office: AI is being deployed to automate a wide range of administrative functions, including appointment scheduling, billing, insurance claims processing, and clinical record management.
- The ROI of Efficiency: For any CFO or operations leader, the financial and efficiency metrics are compelling. AI is not just making things easier; it is generating substantial cost savings.
| Area of Impact | Metric/Statistic |
|---|---|
| AI-Assisted Surgery | Shortens hospital stays by over 20%, saving an estimated $40 billion annually. |
| Medication Errors | Saves an estimated $16 billion by reducing medication dosing errors. |
| Administrative Tasks | Reduces physicians' time spent on administrative work by approximately 20%. |
| Nursing Support | Saves an estimated $20 billion annually through AI nursing assistants that reduce maintenance tasks by 20%. |
| Drug Discovery | Has the potential to cut R&D costs by as much as 70%. |
These figures demonstrate that AI's value is not just clinical but profoundly economic. By automating tedious work—for instance, AI-generated operative reports have been shown to be more accurate (87.3%) than those written by surgeons (72.8%)—AI frees up human capital and financial resources that can be reinvested into direct patient care.

Pillar 3: Personalizing Patient Care and Accelerating Treatment
Beyond improving existing processes, AI is fundamentally changing the nature of treatment itself. It is enabling a shift away from a "one-size-fits-all" model toward a future of hyper-personalized, predictive, and accelerated medicine.
- The Dawn of Personalized Medicine: By analyzing a patient's unique genetic data, lifestyle factors, and complete medical history, AI algorithms can help develop customized treatment plans. A landmark example involved IBM Watson identifying a rare form of leukemia in a patient by analyzing their genetic data against a massive database of medical literature—a feat that would have been impossible for human doctors to accomplish in a timely manner.
- Revolutionizing Drug Discovery: The R&D process for new drugs is notoriously long and expensive. AI is set to change that. By analyzing vast datasets of chemical compounds, AI can predict which are most likely to be effective against a particular disease, potentially slashing drug discovery costs by up to 70%. This is already happening; an AI-discovered drug candidate for Alzheimer's-related psychosis, DSP-0038, progressed from target identification to a Phase I human trial in just one year—a process that traditionally takes many years.
- Improving Patient Outcomes: Ultimately, these advancements translate into better health outcomes. AI systems are being used to identify high-risk hospitalized patients, leading to interventions that can reduce unexpected deaths. In oncology, the use of AI models like Sybil for early lung cancer detection can dramatically increase the five-year survival rate from a grim 10% for late-stage detection to nearly 70% for early-stage detection.
Together, these three pillars form a powerful business case for AI in healthcare. It is a technology that promises to make care more accurate, more efficient, and more effective, addressing the core challenges of quality, cost, and personalization that define the modern healthcare landscape.
3. How Is AI Being Used Today? From the Back Office to the Operating Room
Artificial intelligence is no longer a technology of the future; it is a present-day reality being deployed across the healthcare ecosystem. The most successful and widely adopted applications are not "boil the ocean" projects but rather targeted solutions that solve specific, high-pain, high-cost problems within existing clinical and administrative workflows. These real-world examples make the abstract benefits of AI tangible.
In the Clinic: The Diagnostic Co-Pilot
The clinic is where AI's ability to analyze complex data at superhuman speed is having its most visible impact.
- Medical Imaging Analysis: Companies like Aidoc and Qure.ai have developed "always-on" AI platforms that integrate directly into a hospital's radiology workflow. These systems continuously analyze medical images like CT scans and X-rays in the background, automatically flagging acute, life-threatening abnormalities such as brain hemorrhages or pulmonary embolisms and moving them to the top of the radiologist's worklist. The impact is significant: at one major U.S. medical center, Aidoc's solution helped reduce the average length of an emergency room visit by 59 minutes and cut overall hospitalization time by 18 hours.
- Early Disease Prediction: AI is also moving beyond interpreting acute findings to predicting future disease. The company Mediwhale, for example, has developed a platform that can detect early signs of heart, kidney, and eye diseases simply by analyzing non-invasive retinal scans, potentially replacing the need for blood tests or CT scans. Similarly, pharmaceutical giant AstraZeneca has developed an AI model that can analyze health data to predict with high confidence a patient's risk of developing conditions like Alzheimer's or kidney disease many years in the future.
In the Back Office: The Administrative Powerhouse
The administrative burden in healthcare is immense, and AI is proving to be a powerful tool for automation, creating a foundational layer of efficiency that enables further clinical innovation.
- AI Scribes and Clinical Documentation: This is arguably the most universally adopted AI use case in healthcare today, with some reports indicating that 100% of health systems have some usage of ambient clinical documentation tools. Products like Microsoft's Dragon Copilot and other AI scribes use natural language processing to listen to doctor-patient conversations and automatically generate structured clinical notes. This directly attacks the problem of clinician burnout by freeing doctors from keyboards and allowing them to focus on the patient. This isn't just about saving time; it's about creating higher-quality, structured data that can then be used to train more advanced clinical AI models. If you're interested in applying these concepts to your own systems, learn more about agile software development practices that help operationalize AI rapidly.
- Workflow and Scheduling Automation: AI algorithms are being used to optimize everything from patient appointment bookings to complex nurse schedules. By analyzing patient flow trends, clinician availability, and historical data, these systems can reduce patient wait times, minimize costly no-shows, and prevent staff burnout by creating more balanced schedules.
At the Bedside & Beyond: The Patient Engagement Engine
AI is also changing how patients interact with the healthcare system and manage their own health, extending care beyond the hospital walls.
- Virtual Nursing Assistants: To combat the nursing shortage and reduce administrative load, hospitals are testing AI-powered mobile apps. For instance, Cedars-Sinai is piloting the Aiva Nurse Assistant, an app that handles routine patient requests and administrative tasks, giving nurses more time for hands-on patient care.
- Mental Health Support: With a growing need for mental health services, AI-powered chatbots are emerging as a scalable solution. Apps like Wysa offer 24/7 support for users dealing with stress, anxiety, and depression, using conversational AI to deliver evidence-based techniques like Cognitive Behavioral Therapy (CBT). This is a critical tool, especially as surveys show 20% of U.S. adults are open to using an AI chatbot for mental health support.
- Remote Patient Monitoring (RPM): The proliferation of wearable devices has created a torrent of health data. AI is the key to making this data actionable. RPM platforms like AlayaCare use AI to analyze real-time data from wearables and smart home sensors to monitor patients with chronic conditions like diabetes or heart disease. The AI can predict potential health issues before they become critical, alerting care teams to intervene proactively and ultimately reducing emergency room visits and hospitalizations.
In the Lab: The Research Accelerator
In the high-stakes world of pharmaceutical R&D, AI is dramatically accelerating the pace of discovery.
- Drug Discovery and Clinical Trials: The traditional process of discovering and testing new drugs can take over a decade and cost billions. AI is changing this equation. Platforms from companies like Exscientia and Valence Labs use AI to analyze massive biological and chemical datasets to identify promising drug candidates and predict their effectiveness. Furthermore, AI can optimize clinical trials by identifying specific patient populations who are most likely to respond to a new therapy, as seen in the landmark $5 billion collaboration between Summit Therapeutics and Akeso to develop a next-generation cancer therapy using AI-driven biomarker analysis.
These examples demonstrate a clear pattern: the path to large-scale AI transformation is not a single, monolithic implementation. It is a series of strategic, targeted deployments that solve immediate, tangible problems. This approach—starting with operational AI to clean up data and prove ROI, then leveraging that foundation to build advanced clinical capabilities—is emerging as the most effective roadmap for success.
4. The Big Question: Is AI Replacing Doctors?
No topic generates more debate—or fear—than the idea of AI replacing human clinicians. However, a deep look at the evidence and expert consensus reveals a far more nuanced and collaborative future. The prevailing view within the industry is that AI's role is one of augmentation, not replacement. For a deeper look at workplace impacts beyond healthcare, see our guide on how AI really affects operations and people.
The Verdict: Augmentation, Not Replacement
The most effective framing for AI's role in the clinic is that of a "co-pilot". The AI is the ultimate data-crunching partner, capable of analyzing millions of data points, spotting patterns in scans, and surfacing the latest medical research in seconds. The human clinician remains the "pilot," responsible for exercising judgment, understanding context, showing empathy, and making the final call in partnership with the patient. The conversation in leading medical and technology circles has decisively shifted from "Will AI replace doctors?" to "How will AI, paired with a new generation of clinicians, reshape the healthcare system?". The goal is not to remove the human from the loop but to empower them with insights they can trust and act upon, ultimately making them better at their jobs.
Redefining the Doctor-Patient Relationship
Rather than making the clinician obsolete, AI has the potential to restore the human-to-human connection at the heart of medicine.
- From Typist to Healer: For years, the electronic health record (EHR) has been a source of frustration, often forcing doctors to act as data-entry clerks, staring at a screen instead of engaging with their patients. By automating tedious work like charting and documentation, AI-powered tools like ambient scribes can free the clinician from the keyboard. This recouped time can be reinvested into more quality, face-to-face interaction, allowing for deeper conversations and strengthening the therapeutic relationship.
- Enhanced Shared Decision-Making: AI can also enrich patient consultations. By providing more specific, personalized data about a patient's diagnosis, prognosis, and treatment options, AI can facilitate more meaningful conversations about care. A clinician can use AI-generated insights to better explain the risks and benefits of different paths, empowering the patient to be a more active participant in their own healthcare journey.
- The Patient Perspective: While the potential benefits are clear, patient trust remains a critical factor. Studies show that patients have a clear preference: they trust a human doctor most, followed by a human doctor assisted by an AI system. An AI system acting alone is the least trusted option. This finding underscores the irreplaceable value of the human touch and reinforces the co-pilot model. However, the integration of AI is not without risk. There are valid concerns that it could lead to a more depersonalized, transactional form of care if not implemented thoughtfully.
The key takeaway for any organization implementing AI is that the technology itself is only half the equation. The real challenge—and opportunity—lies in redesigning clinical workflows and incentive structures. The optimistic view is that AI handles administrative tasks, and doctors use the saved time to build stronger patient relationships. However, a more cynical but realistic risk, as highlighted in the AMA Journal of Ethics, is that healthcare systems might simply use that newfound efficiency to pack more appointments into the day, increasing throughput but further eroding the quality of the patient-clinician interaction. Therefore, successful AI implementation is not just a technology project; it is a profound organizational change management challenge that requires a conscious, strategic decision to reinvest the "AI dividend" of saved time back into the human side of medicine.
| Core Task/Capability | The Human Clinician's Role (The "Why") | The AI Co-Pilot's Role (The "How") |
|---|---|---|
| Diagnosis | Final judgment, contextual understanding, communicating the diagnosis with empathy. | Pattern recognition in scans, analyzing lab data, generating differential diagnoses. |
| Treatment Planning | Eliciting patient values, shared decision-making, adapting plans based on patient response. | Analyzing genetic data, predicting drug responses, surfacing evidence-based treatment options. |
| Patient Interaction | Building trust, showing empathy, navigating complex and emotional conversations. | Providing 24/7 chatbot support, sending medication reminders, transcribing conversations for records. |
| Administrative Work | Reviewing, editing, and verifying AI-generated output for accuracy and context. | Automating scheduling, billing, claims processing, and initial documentation. |
This table illustrates the symbiotic relationship. AI handles the quantitative, data-intensive "how," freeing the human clinician to focus on the qualitative, judgment-based "why."
5. Navigating the Hurdles: The Critical Challenges of AI in Healthcare
For all its transformative potential, the path to AI adoption in healthcare is fraught with significant challenges. Acknowledging and proactively addressing these hurdles is not just a matter of compliance; it is essential for building trust, ensuring patient safety, and achieving a positive return on investment. Any organization that ignores these risks does so at its peril.
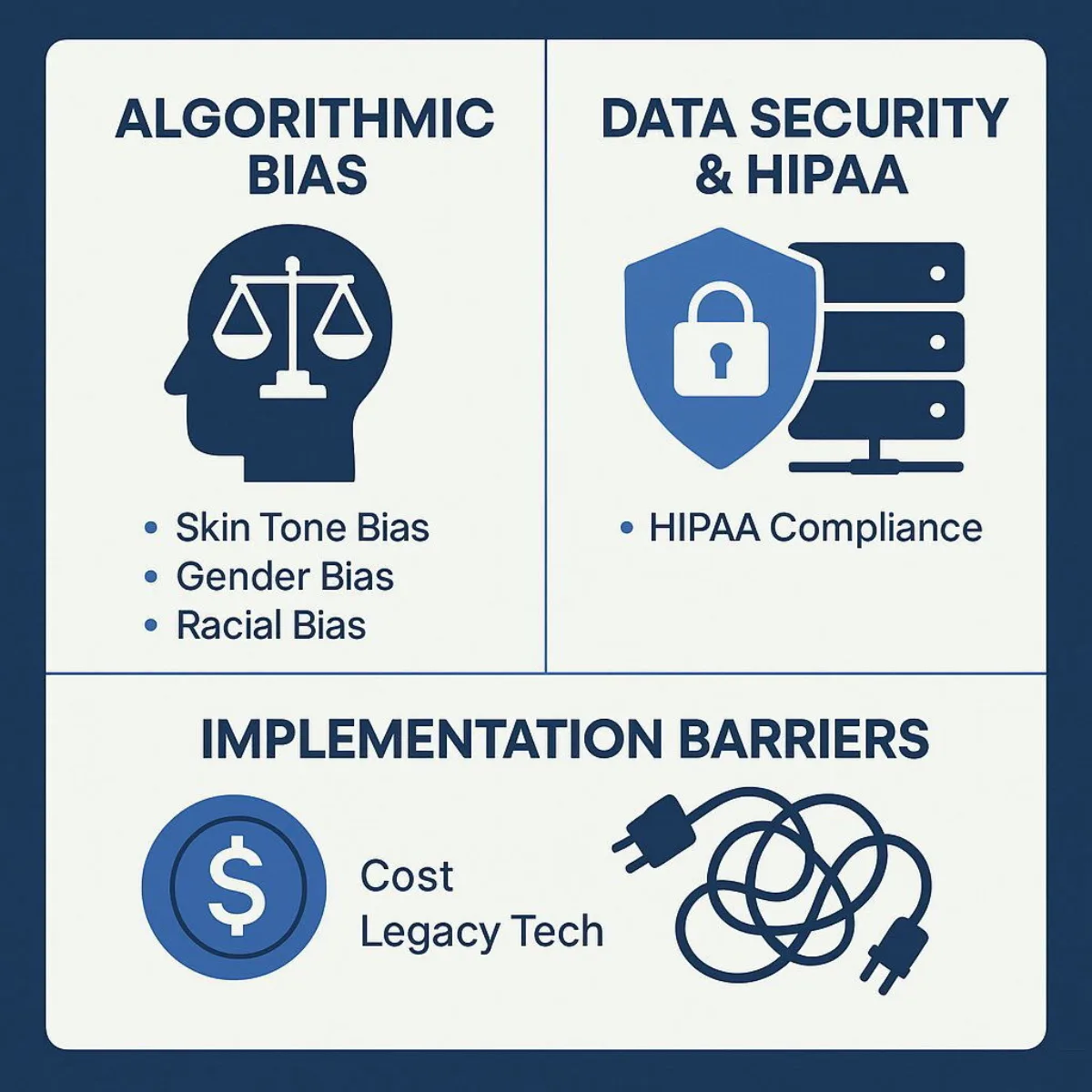
The Bias in the Machine: When AI Inherits Our Flaws
This is one of the most serious ethical challenges facing AI today. AI algorithms are not inherently objective; they learn from the data they are trained on. If that data reflects historical and societal biases, the AI will not only learn those biases but can also amplify them at scale, leading to inequitable care. To understand advanced solutions for minimizing such risks, discover modern approaches like managing non-deterministic AI.
- Real-World Examples of Bias:
- Racial Bias in Risk Prediction: A widely used algorithm in U.S. hospitals was found to be significantly biased against Black patients. It used healthcare spending as a proxy for health needs. Because historically less money has been spent on the care of Black patients, the algorithm systematically underestimated their severity of illness, leading to them being less likely to receive the extra care they needed.
- Skin Tone Bias in Dermatology: Multiple studies have shown that AI tools for diagnosing skin cancer are less accurate for individuals with darker skin tones. This is a direct result of the models being trained predominantly on images of cancerous lesions on lighter skin, creating a dangerous diagnostic blind spot.
- Gender Bias in Cardiology: There are concerns that AI systems could exacerbate the known issue of under-diagnosing cardiac conditions in women, as training data has historically been skewed toward male patients.
- Mitigation Strategies: Combating bias requires a multi-pronged, proactive approach. This includes curating diverse and representative training datasets, implementing technical tools to audit algorithms for performance disparities across demographic groups, building fairness metrics directly into the model's objectives, and, crucially, maintaining a "human-in-the-loop" to provide final oversight and catch biases that the machine may miss.
The Fort Knox Problem: Data Security and HIPAA in the Age of AI
AI systems are data-hungry, often requiring access to vast amounts of sensitive Protected Health Information (PHI). This creates an enormous target for cyberattacks and presents a complex compliance challenge under regulations like the Health Insurance Portability and Accountability Act (HIPAA). Critically, HIPAA's framework was established long before the advent of real-time, cloud-based AI, creating significant gray areas. If you're exploring how secure infrastructure supports modern AI, read our analysis of cloud and data warehouse security.
- Key HIPAA Risk Areas:
- Third-Party Vendors: Many of the most powerful AI tools are cloud-based SaaS platforms. Using them means transmitting PHI outside of an organization's direct control, making rigorous vendor due diligence and ironclad Business Associate Agreements (BAAs) absolutely essential.
- AI Training Data: Using patient data to train AI models is a high-risk activity. If this PHI is not properly encrypted or de-identified according to HIPAA's stringent standards, it can result in massive data breaches and severe regulatory penalties.
- Unintentional Leaks via Public LLMs: A significant and growing risk is staff using public large language models (LLMs) for work-related tasks, such as summarizing patient notes or drafting letters, thereby unintentionally feeding PHI into an insecure, external system.
- Best Practices for Compliance: A "secure-by-design" philosophy is paramount. This involves implementing robust encryption for data both at rest and in transit, strict access controls, and comprehensive audit logs. Organizations should also favor modern AI architectures like federated learning, where models are trained locally on data without the raw data ever leaving the secure environment, or on-device processing, which minimizes data transfer altogether.
The Implementation Mountain: Practical & Financial Hurdles
Beyond the ethical and security concerns lie the practical challenges of implementation.
- Prohibitive Costs: The high initial cost of AI infrastructure, software, and training is a significant barrier to entry, particularly for smaller hospitals and independent practices.
- Legacy System Integration: Healthcare IT is a notoriously complex and fragmented landscape. A new AI tool must be able to integrate seamlessly with existing, often outdated, legacy systems like EHRs. This integration is a major technical and financial hurdle that can derail projects. Explore our guide on legacy software modernization for strategies that can smooth the path.
- Resistance to Change: Healthcare is a field built on established practices and protocols. Clinicians and administrative staff may be resistant to changes in their workflows, viewing new technology with skepticism or as an additional burden. Overcoming this cultural inertia requires careful change management, extensive training, and demonstrating clear value to the end-users.
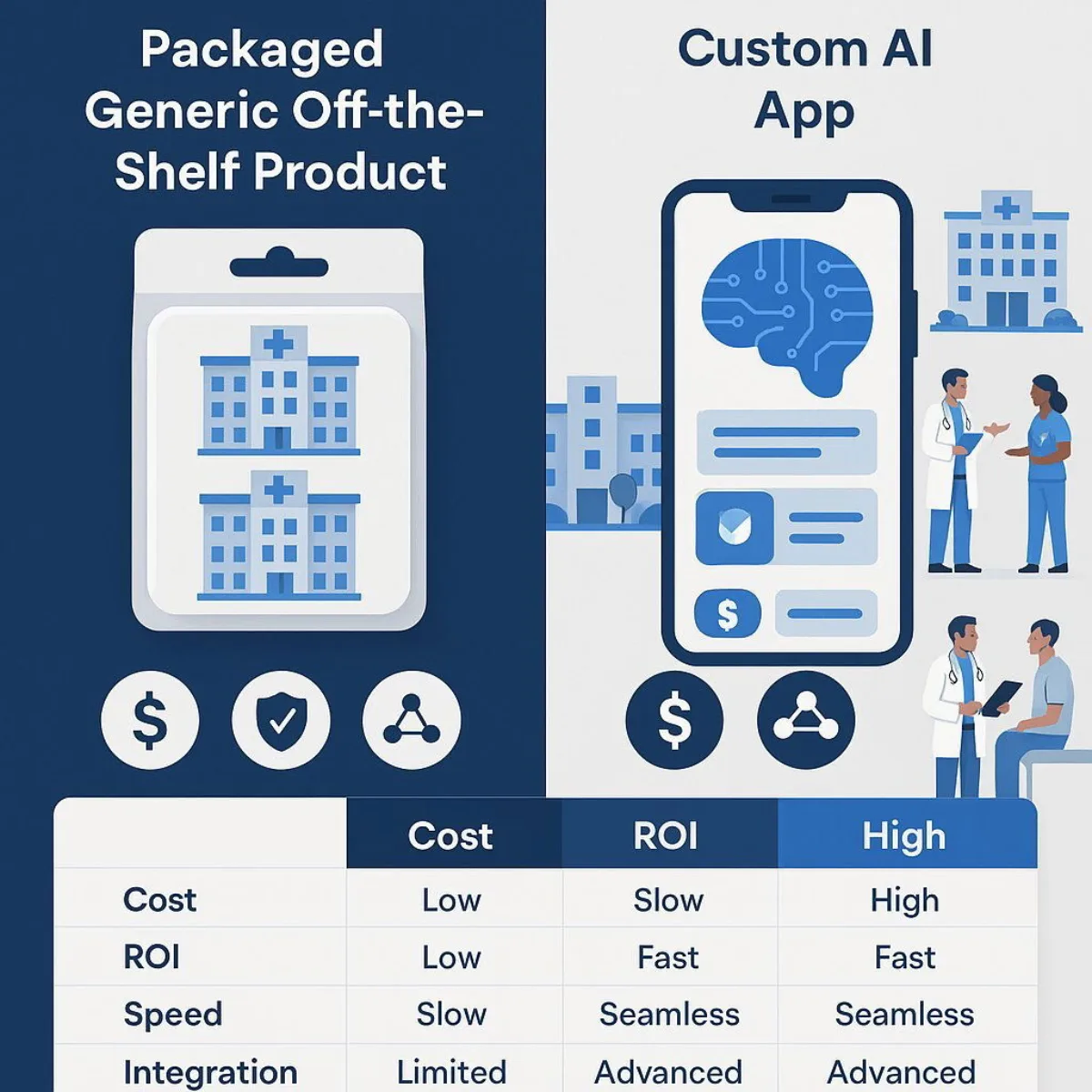
These challenges are not independent silos; they are deeply interconnected. An off-the-shelf AI tool might seem cheaper upfront, but its "black box" algorithm could be impossible to audit for bias. Its cloud data storage practices might create HIPAA compliance headaches. And its generic API might make integration with your specific EHR a nightmare. This complex interplay of challenges makes the choice of technology partner and development approach a critical strategic decision.
6. The Strategic Imperative: Choosing Your Path with Custom vs. Off-the-Shelf AI
For any executive evaluating an investment in healthcare AI, the "buy vs. build" decision is a pivotal one. While off-the-shelf software often appears to be the faster and cheaper path, the unique complexities of the healthcare environment—stringent regulations, legacy systems, and the need for clinical precision—mean that a generic solution can be a short-sighted and ultimately more costly strategy. The decision between a pre-packaged product and a custom-built solution is not merely technical; it is a strategic choice with profound long-term implications for security, scalability, and competitive advantage. For an in-depth comparison of ROI between pricing models, refer to our analysis of software development contract ROI.
The Case for Custom Solutions: The Tailored Tech Advantage
A custom-developed AI solution is designed from the ground up to address the specific challenges and opportunities of your organization. This tailored approach provides critical advantages that are often unattainable with off-the-shelf products.
- Seamless Workflow Integration: Generic software forces you to adapt your processes to its limitations. Custom software is built to fit your unique clinical and administrative workflows, not the other way around. This eliminates friction, boosts user adoption, and maximizes efficiency from day one.
- Unyielding Security and HIPAA Compliance: This is a non-negotiable requirement in healthcare and a key differentiator for custom development. A custom solution can be engineered with a "secure-by-design" philosophy, embedding your specific risk profile, data governance policies, and HIPAA compliance requirements into its core architecture. This provides a far more robust and defensible security posture than the "one-size-fits-all" approach of many off-the-shelf tools.
- Future-Proof Scalability: As your organization grows, adds new services, or adopts new medical technologies, your software must be able to evolve. Custom solutions are built for scalability, allowing you to add features and expand capabilities as your needs change. Off-the-shelf products are often rigid, locking you into a vendor's limited upgrade path.
- True Competitive Differentiation: An off-the-shelf AI tool gives you the same capabilities as every other competitor who buys it. A custom AI application, trained on your proprietary data and tailored to your specific patient population and clinical expertise, becomes a unique strategic asset. It can generate insights and efficiencies that no competitor can replicate, creating a durable competitive advantage.
The Role of Agile Development: Rapid, Adaptive Deployment
The nature of AI development, especially in a dynamic field like healthcare, makes a traditional, linear "waterfall" approach obsolete. AI projects are not static; they are iterative. Models need to be trained, tested, and refined based on real-world feedback from clinicians and administrators. This is where an agile development methodology becomes essential.
An agile approach involves building and deploying the solution in short, iterative cycles or "sprints." This allows a cross-functional team of engineers, clinicians, and stakeholders to collaborate closely, test components in controlled environments, gather immediate feedback, and adapt the plan accordingly. This rapid, adaptive, and transparent process is perfectly suited for the complexities of healthcare AI. It minimizes the risk of building the wrong thing, ensures the final product actually solves the intended problem, and accelerates the time-to-value for the organization.
| Decision Factor | Off-the-Shelf Solution | Custom Solution (The Tailored Tech Advantage) |
|---|---|---|
| Initial Cost | Lower | Higher |
| Long-Term ROI | Potentially lower due to recurring licensing fees, costly workarounds, and inefficiencies. | Potentially higher; often a one-time investment with lower TCO and greater efficiency gains. |
| Deployment Speed | Faster initial setup. | Slower initial build, but can be accelerated with agile methods for faster time-to-value. |
| Integration | Can be challenging; often creates data silos and requires clunky workarounds. | Seamless; designed to integrate perfectly with your specific legacy systems (EHR/EMR). |
| Security & Compliance | Generic, "one-size-fits-all" security that may not meet your specific risk profile. | Bespoke; built from the ground up to your exact HIPAA and data governance requirements. |
| Scalability & Flexibility | Often rigid and limited by the vendor's roadmap. | Highly scalable and adaptable to your organization's future growth and evolving needs. |
| Competitive Differentiation | None; provides the same capabilities as your competitors. | High; creates a unique, proprietary asset that can drive a sustainable competitive advantage. |
This matrix provides a clear framework for the strategic conversation. For organizations that are serious about leveraging AI to solve core challenges and create lasting value, the upfront investment in a custom solution often yields a far greater long-term return.
Conclusion: The Future is Collaborative—Your Next Steps in Healthcare AI
The evidence is clear: Artificial Intelligence is no longer on the horizon of healthcare; it is a present and powerful force of transformation. It is being adopted not as a technological novelty, but as a strategic necessity to combat rising costs, improve clinical accuracy, and manage an overwhelming tide of data. The narrative has matured beyond the fear of replacement to a more sophisticated understanding of AI as a collaborative partner—a co-pilot that augments human expertise, allowing clinicians to focus on the irreplaceable, human-centric aspects of care.
However, this transformation is not without its perils. The path is littered with significant challenges, from the insidious threat of algorithmic bias to the formidable complexities of data security and regulatory compliance. Navigating these hurdles successfully requires more than just a technology-first approach; it demands a holistic strategy that encompasses organizational change, ethical governance, and a clear-eyed view of the risks involved. If you're considering how to future-proof your enterprise operations as the data landscape evolves, our resource on AI-ready cloud data platforms offers practical insights.
For business leaders poised to act, the way forward should be deliberate and strategic. The journey begins not with technology, but with clarity of purpose.
- Assess Your Readiness and Define Your Goal: Before evaluating any tool, start with a clear understanding of the specific, high-pain, high-cost problem you are trying to solve. Is it reducing diagnostic errors in radiology? Slashing administrative time spent on documentation? Improving follow-up care for chronic disease patients? A focused goal is the foundation of a successful AI project.
- Build a Cross-Functional Team: AI implementation is not solely an IT project. Success requires a collaborative team from day one, including clinicians who will use the tool, administrators who understand the workflows, IT experts who can manage integration, and legal/compliance officers who can navigate the regulatory landscape.
- Prioritize Data Governance: Your AI strategy is only as good as your data strategy. Before you can build powerful models, you must have a clean, well-governed, and secure data infrastructure. Getting your data house in order is a critical prerequisite.
- Evaluate Your Technology Path: Use a strategic framework, like the Custom vs. Off-the-Shelf matrix, to determine the right development path for your specific goals. Consider not just the upfront cost, but the long-term implications for security, scalability, and competitive differentiation.
The future of healthcare will be defined by the successful collaboration between human intelligence and artificial intelligence. The organizations that thrive will be those that master this partnership, leveraging technology not to replace their people, but to empower them. For those ready to explore how a tailored, secure, and scalable AI solution can provide a true strategic advantage, the next step is a conversation with experts who understand both the cutting-edge technology and the unique demands of the healthcare domain. At Baytech Consulting, we specialize in crafting these custom solutions, turning the immense potential of AI into tangible, real-world value.
About Baytech
At Baytech Consulting, we specialize in guiding businesses through this process, helping you build scalable, efficient, and high-performing software that evolves with your needs. Our MVP first approach helps our clients minimize upfront costs and maximize ROI. Ready to take the next step in your software development journey? Contact us today to learn how we can help you achieve your goals with a phased development approach.
About the Author

Bryan Reynolds is an accomplished technology executive with more than 25 years of experience leading innovation in the software industry. As the CEO and founder of Baytech Consulting, he has built a reputation for delivering custom software solutions that help businesses streamline operations, enhance customer experiences, and drive growth.
Bryan’s expertise spans custom software development, cloud infrastructure, artificial intelligence, and strategic business consulting, making him a trusted advisor and thought leader across a wide range of industries.


