
How Digital-First Software is Transforming Patient Engagement & ROI in Healthcare
August 18, 2025 / Bryan Reynolds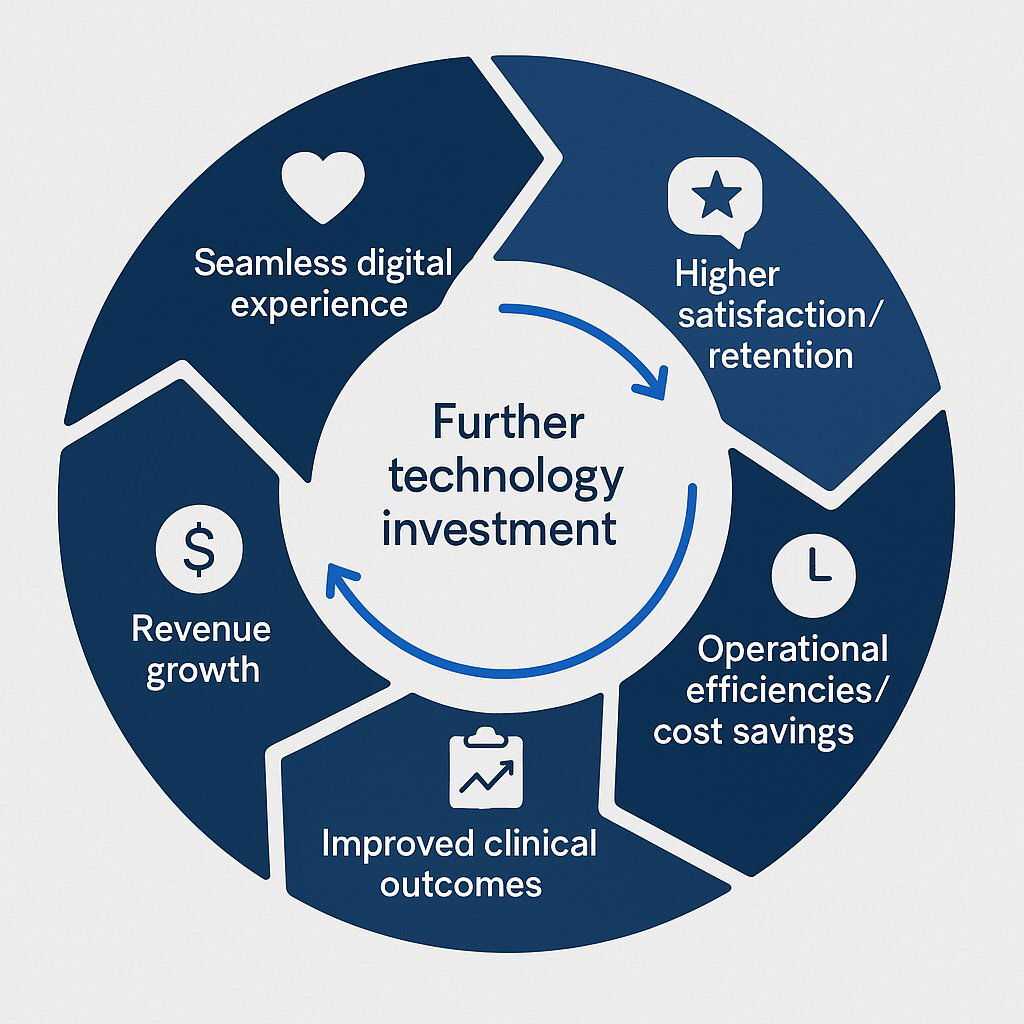
If you're a leader in the healthcare space, you've likely noticed a frustrating paradox. On one hand, patient engagement metrics can be stubbornly low. On the other, those same patients are demanding more—more access, more convenience, more personalization. They expect to manage their healthcare with the same digital ease they use to order groceries, book a flight, or stream a movie. This isn't a contradiction; it's a signal. The disconnect isn't a patient problem; it's a technology and experience problem.
Today’s patients are, first and foremost, consumers. They have been conditioned by every other industry to expect seamless, digital-first interactions. Healthcare is no longer exempt from these expectations. The old models—built on phone calls, paper forms, and inconvenient office hours—are not just outdated; they are actively creating friction that drives patients away. Half of all patients report that a single bad digital experience can ruin their entire relationship with a provider.
This article provides a definitive roadmap for healthcare executives, from the strategic CFO to the visionary CTO, on how to bridge this engagement gap. We will dissect the staggering costs of inaction, explore the new digital demands of the modern healthcare consumer, and detail the specific software solutions that can transform this critical business challenge into your most significant competitive advantage.
The Vicious Cycle: Understanding the True Cost of Low Patient Engagement
Low patient engagement is not a soft problem with vague consequences. It is a direct and quantifiable drain on your organization's clinical outcomes, operational efficiency, and financial health. For executives focused on the bottom line, the numbers paint a stark picture of a vicious cycle where disengagement fuels higher costs, which in turn strains resources and further degrades the patient experience.
The financial bleeding is severe and widespread. Consider medication nonadherence, a classic symptom of poor engagement. When patients don't understand or feel connected to their care plan, they are less likely to follow it. This leads to an estimated $100 billion in otherwise unnecessary medical costs and at least 100,000 preventable deaths in the U.S. each year. The operational drag is just as damaging. Missed appointments, often due to simple forgetfulness or inconvenient scheduling processes, cost the American healthcare industry a staggering
$150 billion annually.
This inefficiency extends deep into acute care. Of the roughly 40 million hospital admissions in the U.S. each year, an estimated 36% are considered preventable—often the result of unmanaged chronic conditions in a disengaged patient population. Worse, once a patient is discharged, the risk skyrockets. An estimated
71% of all hospital readmissions happen because patients neglect their care plans. These readmissions are not only clinically undesirable but also financially punishing, costing an average of
12.4% more than the initial admission ($16,300 versus $14,500).
The costs of disengagement are not static; they compound over time. An analysis of over 30,000 patients found that those with the lowest levels of "activation"—the skills and confidence to manage their own health—incurred costs that were 8% to 21% higher than the most activated patients. The 21% figure is particularly telling, as it represents the cost difference in the
second year , proving that the financial gap widens the longer a patient remains disengaged.
This creates a downward spiral. A disengaged patient is more likely to require a costly, preventable hospital visit. If they have a poor experience during that visit—a common occurrence, with 67% of patients reporting a negative experience —they are highly likely to switch providers. Nearly
40% of patients have left a provider in the last two years due to a poor experience. This churn is a direct hit to revenue, as acquiring a new patient costs five to eight times more than retaining an existing one. The financial link is undeniable: hospitals with "excellent" patient ratings boast an average net margin of
4.7% , a stark contrast to the 1.8% margin for hospitals with lower ratings. For any executive, this means that delaying investment in engagement technology is not a cost-neutral decision. It is an acceptance of escalating future costs and guaranteed revenue erosion.
| Metric | Statistic | Bottom-Line Impact |
|---|---|---|
| Medication Non-Adherence | Costs over $100 billion annually and causes 100,000+ preventable deaths. | Increased treatment costs, higher rates of hospitalization, and poorer long-term outcomes. |
| Missed Appointments | Costs the healthcare industry $150 billion per year. | Lost revenue, inefficient use of provider time, and delays in preventative care. |
| Preventable Readmissions | 71% of readmissions occur due to care plan neglect; cost 12.4% more than initial stay. | Significant direct costs, potential CMS penalties, and inefficient bed utilization. |
| Low Patient Activation | Least-activated patients cost 8% to 21% more than highly-activated patients. | Higher overall cost of care per patient, indicating systemic inefficiencies. |
| Patient Churn | 50% of patients say one bad digital experience ruins the relationship. | High patient acquisition costs, loss of lifetime patient value (estimated at $1.4M per loyal patient ), and damaged reputation. |
The New Healthcare Consumer: What Today’s Patients Demand
The root cause of this engagement crisis is a fundamental and irreversible shift in patient expectations. The modern patient is a digital consumer, and they are bringing the same demands for convenience, transparency, and self-service from retail and banking directly into the healthcare arena. For healthcare organizations, meeting these demands is no longer optional; it is the primary driver of patient acquisition and retention.
Digital access is now a key factor in a patient's choice of provider. A stunning 59% of millennials report they would switch doctors for one with better online access. This sentiment is not limited to younger generations;

24% of all consumers are willing to switch providers to get access to virtual visit options. The ability to book, change, or cancel appointments online is a powerful draw, with
68% of people saying they are more likely to choose a provider who offers this capability.
The patient journey itself has been completely redefined. It no longer begins with a phone call to the front desk; it begins with a search engine. An overwhelming 83% of adult internet users go online to research health-related queries , and
77% start their search for a new physician by reading online reviews. This means a provider's digital presence—its website, its reviews, its online scheduling tools—is its new front door. A poor digital experience can stop a potential patient from ever making contact.
This shift has ignited an explosion in the market for patient engagement technologies. The U.S. market alone is projected to surge from $5.16 billion in 2021 to over $105 billion by 2033, a compound annual growth rate of nearly 20%. The demand for telehealth, which spiked during the pandemic, has stabilized at a new, much higher baseline, accounting for
17% of all outpatient visits in 2023—a massive leap from just 0.1% pre-pandemic.
Ultimately, patients now expect their healthcare interactions to mirror the seamless experiences they have with retail giants. Sixty percent of consumers explicitly state this expectation. The stakes are incredibly high, as
50% of patients say a single bad digital experience is enough to ruin their entire relationship with that provider. The implication for marketing directors and heads of sales is profound: your digital platform is not an IT expense. It is a core marketing and patient acquisition channel, as vital to your brand and revenue as your physical facilities. The digital experience is the patient experience.
The Digital Toolkit: Four Categories of Software to Revolutionize Patient Engagement
Understanding the problem and the patient's demands is the first step. The second is deploying the right technology to solve it. A modern patient engagement strategy is built on a foundation of four interconnected software categories. Each serves a distinct purpose, but together they create a seamless, personalized, and continuous care experience that drives both patient satisfaction and operational excellence.
1. The Digital Front Door: Patient Portals & Communication Hubs
The patient portal is the cornerstone of a digital engagement strategy. It acts as a secure, centralized online hub where patients can manage every non-clinical aspect of their healthcare journey. To be effective, however, a portal must be more than a simple administrative tool. While core functions like online appointment booking (preferred by 43% of patients ), secure messaging with providers, access to lab results, and online bill pay are essential, they are merely table stakes.

True engagement is driven by features that empower the patient and integrate directly into their care. This includes access to personalized educational resources tailored to their specific condition, interactive tools that aid in shared decision-making, and seamless integration with the provider's Electronic Health Record (EHR). A portal that only offers basic administrative functions will fail to capture patient interest and will see low adoption rates. Furthermore, success is heavily dependent on provider buy-in. Studies consistently show that patients are significantly more likely to register for and actively use a portal when their physician recommends it and incorporates it into the clinical workflow.
Building a portal that acts as a true communication hub rather than another data silo requires deep integration expertise. At Baytech Consulting, we leverage secure, scalable cloud platforms like Microsoft Azure to build these solutions. This ensures robust interoperability between the portal and disparate backend systems—like EHRs, billing software, and lab systems—creating a single, unified source of truth for the patient.
2. Care in Your Pocket: The Rise of mHealth Applications
While a portal serves as the web-based hub, a mobile health (mHealth) app puts the power of engagement directly into the patient's pocket. These apps extend care beyond the clinic, providing tools for self-management, continuous monitoring, and on-the-go communication.
Key features of a successful mHealth app include symptom checkers, medication reminders, and customizable health dashboards that allow patients to track key metrics like blood pressure or fitness goals. The impact of these features is tangible: simple smartphone notifications have been shown to increase medication adherence by
34-38% . A critical trend is the integration with wearable devices. With
50% of wearable users already sharing data with their doctors, an mHealth app that can sync with smartwatches and fitness trackers provides a rich, real-time stream of health data that can inform care plans and enable early interventions.
For an mHealth app to succeed, the user experience (UI/UX) must be flawless. A simple, intuitive, and clutter-free interface is essential for ensuring adoption across all age groups and technical abilities. A confusing or poorly designed app will be quickly abandoned.
Delivering this seamless experience requires a high-performance, scalable backend. This is where our Rapid Agile Deployment and engineering excellence come into play. We utilize modern architectural patterns, using technologies like Docker to containerize application services and Kubernetes to orchestrate them. This approach ensures that the application is resilient, scalable, and can handle a growing user base and massive volumes of data without sacrificing performance or reliability.
3. Bridging Distances: Telehealth and Remote Patient Monitoring (RPM)
Telehealth and RPM platforms have fundamentally changed how and where care can be delivered. They provide unparalleled convenience, improve the management of chronic diseases, and allow for proactive interventions by monitoring patients outside the traditional clinical setting.
A robust telehealth platform must include HIPAA-compliant video and audio consultations, secure messaging capabilities, and deep integration with the provider's EHR and scheduling systems. RPM takes this a step further by enabling the electronic transmission of clinical data from medical devices at the patient's home—such as blood pressure cuffs, glucose meters, or even pacemakers—directly to the care team. The demand for these services is exploding, with the number of U.S. patients using RPM tools projected to reach
30 million by 2024.
The clinical results are compelling. RPM has been proven to improve outcomes for patients with chronic conditions like diabetes and heart failure. A landmark example is Ochsner Health's "Connected MOM" program, which uses RPM to monitor high-risk pregnancies. By providing patients with digital blood pressure cuffs and scales, the program enables the care team to detect dangerous complications like hypertensive disorders earlier, all while reducing the need for burdensome in-person visits.
The security and integrity of this transmitted health data are non-negotiable. Building these platforms requires a deep understanding of data security protocols. We build our telehealth and RPM solutions on powerful, secure databases like PostgreSQL . Its advanced features, including robust encryption for data in transit and at rest, granular role-based access controls, and comprehensive auditing capabilities, provide the foundation needed to ensure full HIPAA compliance and protect sensitive patient information.
4. The Intelligence Layer: AI and Predictive Analytics for Hyper-Personalization
The final and most transformative layer of a modern engagement strategy is the use of Artificial Intelligence (AI) and predictive analytics. This is what allows a healthcare organization to move from a reactive, one-size-fits-all approach to a proactive, predictive, and hyper-personalized model of care.
AI algorithms can analyze vast datasets—including EHR data, demographics, and patient behavior patterns—to tailor every aspect of the patient journey. Instead of generic appointment reminders, AI can send personalized messages that resonate with an individual's specific health goals and communication preferences. This moves engagement from a transactional process to a relational one.
The true power lies in prediction. AI models can identify which patients are at the highest risk of missing appointments, failing to adhere to their medication regimen, or being readmitted to the hospital. This allows care teams to intervene before a negative event occurs. Geisinger Health System, for example, uses a predictive AI model to identify chronic disease patients at high risk of admission, a strategy that has led to a
10% reduction in avoidable emergency department visits and hospitalizations.
Beyond clinical applications, AI drives significant operational efficiency. AI-powered chatbots and virtual assistants can handle routine patient inquiries, automate the appointment scheduling process, and intelligently triage patient needs, freeing up staff to focus on more complex care and reducing administrative burnout. It's estimated that AI-driven chatbots will save healthcare organizations
$3.6 billion globally by automating these tasks.
Implementing an effective AI layer is not about simply plugging in a tool. It requires a sophisticated and unified data strategy. This is the essence of our Tailored Tech Advantage . We don't just deploy an AI model; we architect the underlying data infrastructure. By leveraging platforms like Azure Health Data Services , we break down the data silos that plague most healthcare organizations, creating the clean, integrated, and high-quality data streams that are essential for fueling accurate, reliable, and powerful AI insights.
| Feature | Patient Portal | mHealth App | Telehealth/RPM | AI/Analytics Layer |
|---|---|---|---|---|
| Online Appointment Scheduling | ● | ● | ● | ● |
| Secure Provider Messaging | ● | ● | ● | |
| Lab Result & Record Access | ● | ● | ||
| Online Bill Pay | ● | ● | ||
| Medication Reminders | ● | ● | ● | |
| Wearable Device Integration | ● | ● | ● | |
| Live Video Consultations | ● | ● | ● | |
| Remote Vitals Monitoring | ● | ● | ||
| Personalized Health Education | ● | ● | ● | |
| Symptom Checkers | ● | ● | ||
| Predictive Risk Scoring | ● |
The Strategic Crossroads: Building a Custom Solution vs. Buying Off-the-Shelf
Once you've committed to investing in patient engagement technology, you face a critical strategic decision: do you buy a pre-built, off-the-shelf (OTS) solution, or do you partner with a firm like Baytech Consulting to build a custom software platform? While OTS vendors promise speed and lower upfront costs, a deeper analysis of Total Cost of Ownership (TCO) and long-term strategic value reveals that a custom solution is often the superior investment for forward-thinking healthcare organizations.
OTS software offers the allure of rapid implementation, sometimes in as little as two to six weeks, with a lower initial price tag. This can be a viable option for smaller clinics with standard workflows and an urgent need to get a basic system in place. However, this initial convenience comes with significant long-term trade-offs. The OTS model is built on recurring subscription and licensing fees that accumulate year after year. Customization is highly limited, forcing your organization to conform its unique clinical workflows to the rigid structure of the software. Integration with your existing systems (EHR, billing, labs) is often clunky and incomplete, with some vendors charging exorbitant fees for API access or simply not supporting the integrations you need. These hidden costs and workarounds can inflate the total implementation cost by as much as
40% . Perhaps most telling is that an estimated
85-90% of features in typical OTS products go completely unused, meaning you are paying a premium for bloated software that doesn't fit your needs.
A custom software solution requires a larger upfront investment—a custom healthcare app can range from $75,000 to over $250,000—and a longer development timeline of six to twelve months or more. However, this initial investment buys you complete ownership and control. There are no perpetual licensing fees. Every feature is designed and built to support
your specific workflows, not a generic industry template. This results in a streamlined, intuitive system that boosts staff adoption and efficiency. Most importantly, a custom solution is built with interoperability at its core, ensuring seamless data flow between all your critical systems. Over a three-to-five-year horizon, the TCO for a custom solution is often significantly lower than for an OTS product burdened by recurring fees and costly workarounds.
This decision transcends a simple cost analysis; it's about whether you view technology as a utility or as a strategic, moat-building asset. In the new era of value-based care, differentiation is paramount. An OTS solution, by its very nature, is a commodity available to all your competitors. A custom platform, however, allows you to codify your unique care delivery models, proprietary clinical pathways, and signature patient experience directly into your technology. It transforms your software from a mere operational tool into a durable competitive advantage that cannot be easily replicated by others.
The valid concerns around the higher upfront cost and longer timeline of custom development are precisely why we founded Baytech Consulting on two core principles: our Tailored Tech Advantage and Rapid Agile Deployment . Our Tailored Tech Advantage means we don't just build software; we architect a strategic asset that is meticulously crafted to maximize your operational efficiency, enhance your unique brand of care, and deliver a superior patient experience. Simultaneously, our Rapid Agile Deployment methodology directly mitigates the timeline and budget risk associated with large-scale projects. By working in short, iterative cycles (sprints), we deliver functional pieces of the application early and often. This transparent process keeps you involved at every stage, allows for flexibility as needs evolve, and ensures the project delivers continuous value while staying on track and on budget.
| Factor | Off-the-Shelf Solution | Custom Solution (The Baytech Way) |
|---|---|---|
| Initial Cost | Lower upfront investment. | Higher upfront investment. |
| Total Cost of Ownership (3-5 Yrs) | Higher due to recurring license fees, upgrade costs, and paid customizations. | Lower, with a one-time development cost and predictable maintenance. No license fees. |
| Workflow Alignment | Forces you to adapt your unique workflows to the software's rigid structure. | Software is built around your exact clinical and administrative workflows for maximum efficiency. |
| Integration & Interoperability | Often limited, clunky, or requires expensive add-ons. Can create new data silos. | Built for seamless integration with your existing EHR, billing, and lab systems from day one. |
| Scalability & Future-Proofing | Limited by the vendor's roadmap and pricing tiers. You don't control your future. | Infinitely scalable and adaptable. You own the codebase and can evolve the platform as your needs change. |
| Data Security & Compliance | Relies on the vendor's security posture; you have limited control and visibility. | Security protocols are tailored to your specific needs, providing superior control and peace of mind for HIPAA compliance. |
| Competitive Differentiation | Commodity tool available to all your competitors. Offers no unique advantage. | Creates a proprietary, defensible asset that codifies your unique value proposition into the patient experience. |
| Vendor Dependency | High. You are locked into their ecosystem, pricing, and support model. | Zero. You own the software and control its destiny. Supported by a dedicated team that knows your system intimately. |
From Engagement to Earnings: The Tangible ROI of a Patient-Centric Strategy

Investing in a modern, patient-centric software platform is not a cost center; it is one of the highest-return initiatives a healthcare organization can undertake. The return on investment (ROI) manifests across the entire enterprise, driving down costs, increasing revenue, and creating a virtuous cycle of continuous improvement.
The cost savings are immediate and substantial. Engaged patients, who are active partners in their care, are 30% less likely to be readmitted to the hospital after a discharge. Technology-driven engagement strategies, such as telehealth and remote monitoring, have been shown to reduce costly emergency department visits by up to
43% . The Atrium Health "Hospital at Home" program, a model built on virtual care and RPM technology, has saved the health system nearly
30,000 inpatient bed days since its inception—a massive operational and financial win.
On the revenue side, the impact is equally profound. A loyal patient, nurtured by positive and seamless experiences, has an estimated lifetime value to a health system of $1.4 million . The leverage here is enormous: increasing patient retention by just
5% can boost practice profitability by 25% to 100% .
These financial gains are fueled by dramatic improvements in operational efficiency. Automating routine administrative tasks like appointment scheduling, reminders, and billing frees up hundreds of hours of staff time, allowing them to focus on higher-value, direct patient care. Technology that empowers patients to self-serve can reduce a nurse's time spent on delegable tasks by
10-16% .
Case studies prove the power of this model. Concert Health provides integrated behavioral healthcare by embedding virtual therapists into primary care practices. Their technology platform, which facilitates communication, scheduling, and progress tracking, is core to their model. The results are phenomenal: 85% of patients referred to the program actively engage in care, and they see a 50% reduction in depression and anxiety symptoms within 90 days. This is a perfect example of how a tech-enabled strategy drives superior engagement, which in turn produces superior clinical and financial outcomes.
This ROI is not a simple, linear calculation. It is a self-perpetuating flywheel. A strategic investment in seamless digital tools improves the patient experience. This leads to higher satisfaction scores and better online reviews, which in turn drives new patient acquisition. Simultaneously, higher engagement leads to better medication adherence and self-management, which improves clinical outcomes and reduces costly events like readmissions. The combination of lower costs and higher revenue improves the organization's margins, freeing up capital that can be reinvested into even better technology, which further accelerates the flywheel and widens the competitive gap between your organization and those stuck in the old model.
AI-powered healthcare solutions, for example, have become a catalyst for these improvements, driving market growth while helping organizations optimize patient outcomes and costs.
Conclusion: Your Next Steps Toward a Future-Proof Healthcare Experience
The evidence is clear and overwhelming. Low patient engagement is a direct symptom of an outdated, high-friction digital experience that fails to meet the expectations of the modern consumer. The solution is not to incrementally fix broken analog processes, but to make a strategic investment in a modern software ecosystem that delivers the convenience, personalization, and access that patients now demand.
This investment is not an expense to be minimized, but a high-ROI strategy that ignites a powerful flywheel of better clinical outcomes, lower operational costs, and sustainable revenue growth. While off-the-shelf products offer a quick fix, the most strategic and financially sound path for forward-thinking organizations is a custom-built solution. A tailored platform transforms your technology from a simple utility into a core strategic asset, codifying your unique value proposition and creating a durable competitive advantage.
For executives ready to lead this transformation, the path forward involves three clear steps:
- Audit Your Digital Friction: Begin by meticulously mapping your current patient journey, from the moment a person searches for care online to their final payment. Identify every point of friction, every analog dead-end, and every clunky process. Where do patients drop off? Where are they forced to pick up the phone or fill out a paper form? This audit will reveal your biggest opportunities for improvement. If you’re not sure where to start, our UX design experts can help identify key friction points in your patient experience.
- Define Your Business Objectives: Don't start by creating a list of software features. Start by defining your strategic goals. Do you need to reduce patient no-shows by 15%? Increase market share in a key demographic? Improve medication adherence for a specific chronic disease population? Your business objectives must drive your technology strategy, not the other way around. For more ideas on aligning tech and business goals, see our guide on digital transformation across industries.
- Evaluate Your Strategic Path: With your goals clearly defined, you can honestly assess the build-vs-buy decision. Can a generic, one-size-fits-all tool truly achieve your specific strategic objectives and align with your unique clinical workflows? Or is a tailored, custom-built solution the necessary investment to secure a long-term competitive edge? To weigh this choice with a clear ROI lens, explore our software ROI framework.
Building a truly engaging and differentiated patient experience is a complex but achievable goal. It requires a partner with deep engineering expertise, a nuanced understanding of the healthcare landscape, and a commitment to building strategic assets, not just writing code.
If you're ready to move beyond the generic and build a technology platform that will delight your patients and power your growth for the next decade, our team is here to help. Let's schedule a conversation to discuss how a tailored software solution from Baytech Consulting can transform your patient engagement strategy.
Further Reading & Resources
- https://www.oecd.org/en/publications/patient-engagement-for-patient-safety_5fa8df20-en.html
- https://www.ama-assn.org/system/files/future-health-case-study-atrium-health.pdf
- https://www.hyro.ai/blog/measuring-roi-on-digital-patient-experience-initiatives/
About Baytech
At Baytech Consulting, we specialize in guiding businesses through this process, helping you build scalable, efficient, and high-performing software that evolves with your needs. Our MVP first approach helps our clients minimize upfront costs and maximize ROI. Ready to take the next step in your software development journey? Contact us today to learn how we can help you achieve your goals with a phased development approach.
About the Author

Bryan Reynolds is an accomplished technology executive with more than 25 years of experience leading innovation in the software industry. As the CEO and founder of Baytech Consulting, he has built a reputation for delivering custom software solutions that help businesses streamline operations, enhance customer experiences, and drive growth.
Bryan’s expertise spans custom software development, cloud infrastructure, artificial intelligence, and strategic business consulting, making him a trusted advisor and thought leader across a wide range of industries.


